Modern ideas about the treatment of regurgitation syndrome in children of the first year of life
Proper and rational nutrition of a child in the first year of life largely determines his health in the future. This is especially true for children with any illnesses.
A fairly common problem in children of the first year of life is functional disorders of the gastrointestinal tract. They are associated with changes in motor function and somatic sensitivity, with deviations in the secretory and absorption functions of the digestive system [1]. Regurgitation syndrome occupies a significant place among these disorders. Regurgitation syndrome refers to the reflux of stomach contents into the oral cavity. In this case, unlike vomiting, regurgitation of gastric contents occurs passively, without tension of the abdominal press and diaphragm, and is not accompanied by autonomic reactions (hypersalivation, pale face, tachycardia, cold extremities). The high frequency of regurgitation in children of the first year of life is due to anatomical and physiological characteristics: the structure of the upper gastrointestinal tract, the immaturity of the neurohumoral component of the sphincter apparatus and imperfect motility of the gastrointestinal tract.
Regurgitation, which in some cases is observed in healthy newborns, is not in itself a sign of any disease [2]. Persistent regurgitation in children in the first year of life may be associated with weakness of the lower esophageal sphincter and abnormal motility of the esophagus, which lead to spontaneous reflux of gastric contents into the esophagus.
Regurgitation in children of the first year of life can occur without organic changes in the gastrointestinal tract, as well as against their background.
Organic changes leading to regurgitation are:
- pyloric stenosis;
- malformations of the gastrointestinal tract [3]. Regurgitation without organic changes in the gastrointestinal tract:
- rapid sucking, aerophagia, overfeeding, violation of feeding schedule, inadequate selection of formulas, etc.;
- perinatal damage to the central nervous system (CNS);
- early transition to thick foods;
- pylorospasm.
According to modern concepts, the intensity of regurgitation is assessed on a five-point scale, reflecting the frequency and volume of regurgitation (Table 1).
Persistent regurgitation can be a manifestation of both pathological gastroesophageal reflux (GER) and gastroesophageal reflux disease (GERD). If physiological regurgitation is usually observed during wakefulness, then pathological regurgitation most often occurs when the child is in a horizontal position. Increased secretion of gastric juice and constant reflux into the esophagus can lead to the development of esophagitis. Clinical manifestations that suggest the development of esophagitis are dysphagia, anorexia, crying, restless behavior during feeding or sleep. This group of children often experience various bronchopulmonary complications and night cough.
In addition to the clinical picture, laboratory and instrumental examination methods are also of great importance for the diagnosis of regurgitation. In some cases, only with their help can a correct diagnosis be made and further treatment tactics determined.
24-hour intraesophageal pH-metry. It is the most informative method for this disease. This method allows you to identify the total number of reflux episodes, their duration, and the level of acidity in the esophagus. According to pH-metry, with functional regurgitation (regurgitation), the pH in the distal esophagus can be below 4, but not more than 1 hour daily (less than 4% of the total monitoring time); with GER, the pH in the distal esophagus reaches 4, exceeding 4 .2% of the total monitoring time, and in case of pathological reflux its duration exceeds 5 minutes [4].
- Esophagogastroduodenoscopy (EGD) with targeted biopsy of the esophageal mucosa. This examination allows you to assess the nature of the mucous membrane, the consistency of the cardiac sphincter, etc. Histological examination allows you to determine the severity of the inflammatory process as early as possible.
- Esophagotonokymography. Allows you to analyze the tone of the lower esophageal sphincter and the state of motor function of the stomach, the amplitude of contractions.
- Scintigraphy. Allows you to evaluate the slowdown of esophageal clearance.
- Radiography. It is a method that allows you to diagnose a pathology such as hiatal hernia, which is the cause of persistent regurgitation and vomiting.
The lack of timely and correct treatment, primarily dietary correction, for this pathology can lead to pronounced changes in the health status of children:
- violation of mass growth indicators;
- reflux esophagitis;
- Iron-deficiency anemia;
- aspiration pneumonia;
- sudden death syndrome.
Treatment of regurgitation . Treatment of regurgitation in infants should be consistent and include a set of measures:
- conducting postural therapy;
- diet therapy, use of thickeners;
- use of drug therapy:
– prokinetics, – H2-histamine receptor blockers, – proton pump inhibitors;
- surgical methods of treatment.
At the same time, psychological support and explanatory work carried out by the doctor with parents are of no small importance. This primarily helps to assess the effectiveness of the prescribed treatment, since an adequate assessment of the frequency and volume of regurgitation largely depends on the parents’ correct understanding of the situation and the degree of their emotional comfort.
Postural therapy (changing the position of the child's body) is aimed at reducing the reflux of gastric contents into the esophagus and should be carried out during the day, as well as at night. Feeding the baby should occur in a sitting position, at an angle of 45-60°C. Holding the baby after feeding should be at least 20–30 minutes.
A significant place in the treatment of regurgitation belongs to a highly effective method - diet therapy. The choice of diet therapy depends on the type of feeding the child is on.
If you are breastfeeding, you should continue breastfeeding. It should be remembered that even persistent regurgitation is not an indication for transferring a child to mixed or artificial feeding. To successfully treat regurgitation, it is necessary to create a calm environment for the mother and normalize the child’s feeding regimen, excluding overfeeding or aerophagia. Regurgitation and GER can be manifestations of food intolerance. In this case, the mother should be prescribed a hypoallergenic diet.
If regurgitation is a consequence of hypertension or neurological disorders, diet therapy should be combined with drug treatment prescribed by a pediatric neurologist or neonatologist.
In case of persistent regurgitation or lack of effect from the therapy, it is permissible to use breast milk thickeners (for example, “BIO-Rice broth”. For children over 1–2 months, it is permissible to use denser food - dairy-free rice porridge, added in the amount of 1 teaspoon. Presence of a thickener provides a greater viscosity of the mixture, as a result of which it stays in the stomach longer. This leads to swelling of the contents of the stomach and an increase in the pressure of the food gruel on the muscular sphincter at the outlet of the stomach, which promotes its opening. The effect of gravity on the bolus of food prevents it from being thrown back out of the stomach into the esophagus, and all this together leads to the normal progressive movement of food through the digestive tube and the cessation of regurgitation.
If by three months of life regurgitation does not disappear or its number does not decrease, then the child needs additional examination to determine the causes of regurgitation and the prescription of the necessary drug therapy.
Artificial feeding . In this case, it is also necessary to evaluate the child’s diet: the volume and quality of the artificial formula used. The child should receive an adapted milk formula in a volume appropriate for his age.
If there is no effect from the main measures (postural therapy, establishment of a feeding regimen), it is necessary to decide on the appointment of a specialized antireflux mixture [5, 6]. A feature of this group of mixtures is the presence of a thickener in their composition, which increases their viscosity.
Depending on the type of thickener, anti-reflux mixtures are divided into two groups:
- Containing carob gum (“Nutrilon antireflux”, “Frisov 1”, “Frisov 2”, “Nutrilak AR”, “Humana AR”)
- Containing rice starch (“Samper Lemolak”, “Enfamil AR”) (
).
The content of locust bean gum in mixtures should not exceed 1 g per 100 ml of the finished product. In the products presented in the table, the gum content ranges from 0.34 to 0.6 g per 100 ml.
The ratio of whey protein to casein in the mixture is also of certain importance. It is known that casein in the stomach forms a denser clot and enhances the effect of the thickener (locust bean gum or starch). Similar casein-predominant mixtures are “Nutrilon antireflux” and “Enfamil AR”.
When choosing an antireflux mixture, a differentiated approach should be used. The most pronounced clinical effect is observed when using mixtures containing gum. They can be recommended either in full or partially, as a replacement for part of the feeding. In this case, the amount of mixture needed by the child is determined by the onset of the therapeutic effect. The duration of use of these mixtures is on average 3–4 weeks.
Artificial mixtures containing starch as a thickener act “softer”. They are indicated for children with mild forms of regurgitation (1–3 points) both with normal stool and with a tendency to unstable stool. They are recommended to be prescribed to completely replace the previously obtained mixture. The duration of their use is somewhat longer than when using gum-containing artificial mixtures.
When prescribing an antireflux mixture, it should be remembered that this group of mixtures is only part of the treatment of the disease and is recommended by a doctor. The use of antireflux formulas in healthy children who do not regurgitate is not recommended.
Drug therapy . If diet therapy is ineffective, drug therapy is prescribed, combined with the continued use of a therapeutic antireflux mixture. The prescribed groups of medications include the following:
1. Antacids (Phosphalugel, Maalox). These drugs are prescribed in a dose of 1/4 sachet or 1 teaspoon after each feeding - for children under 6 months; 1/2 sachet or 2 teaspoons after each feeding - children 6–12 months. The course of treatment is 10–21 days.
2. Prokinetics:
– metoclopramide (Cerucal, Reglan); – cisapride (Prepulsid, Coordinax); – domperidone (Motilium).
The course of treatment with prokinetics is 10–14 days. They are prescribed at a dose of 0.25 mg/kg - 3-4 times a day 30-60 minutes before meals. However, one should remember the side effects of this group of drugs, which limit their use in pediatric practice. Metoclopramide drugs have a pronounced central effect (pseudobulbar disorders have been described) and are not recommended for use in infants with regurgitation syndrome. When using cisapride drugs, prolongation of the QT interval in children has been described, which serves as a limitation on the use of such drugs. In practice, the best results and minimal side effects are obtained by the drug Motilium (domperidone), produced in a convenient form for giving to young children - in syrup. The drug affects intestinal motility and, thus, accelerates the passage of both gastric and intestinal contents, which leads to faster gastric emptying and, accordingly, to the absence of regurgitation.
3. H2 receptor blockers. They are the drugs of choice in the presence of pathological GER, manifested by regurgitation. Recommended doses: Ranitidine 5-10 mg/kg per day, Famotidine 1 mg/kg per day. Duration of treatment is up to 3 months with gradual withdrawal of drugs.
Thus, regurgitation syndrome in children of the first year of life is a common problem. Diet therapy plays a significant role in the treatment of these conditions. Adequate and timely recommendations for feeding a child with regurgitation syndrome avoid possible complications and ensure normal growth and development of the child.
For questions regarding literature, please contact the editor.
E. A. Gordeeva , Candidate of Medical Sciences T. N. Sorvacheva , Doctor of Medical Sciences RMAPO , Moscow
Why does a newborn spit up?
In most cases, the process is caused by the digestive characteristics of the infant and the immaturity of the internal organs: in the first months of life, the muscular sphincter at the border of the esophagus and stomach, which holds food, has not yet developed.
This anatomical feature is typical for all babies, so the likelihood of regurgitation is the same when breastfed or bottle-fed.
But how often and how much a newborn burps depends on various conditions: intrauterine development and childbirth, full-term birth, heredity, intensity of gas formation and colic, health status and largely on how well the feeding is going.
Some parents themselves unintentionally “force” their baby to burp.
The following can lead to the backflow of consumed milk or formula:
- supplementary feeding above the age norm;
- feeding not according to the schedule;
- air bubbles in the bottle;
- suboptimal attachment to the breast;
- unsuitable mixture;
- complementary feeding too early;
- feeding a child when he is excited and crying;
- pressure on the child’s tummy soon after eating, sudden turning over, change in body position;
- massage, active games after meals.
The combination of physiological characteristics and the listed reasons creates a problem. This can be avoided. But if a child burps after feeding for no apparent reason, it is important for mom and dad to look at the volume and time of regurgitation, and most importantly, pay attention to how the baby feels and gains weight.
Does the mixture affect regurgitation?
Spitting can be caused by an allergy to cow's milk protein in the formula, increased gas production, or spoiled or inappropriate formula. Goat milk formulas are easier to digest, reducing the severity of flatulence and the risk of regurgitation. As for antireflux mixtures, they are medicinal.
Until what age does a newborn spit up?
If a child spits out up to 3-5 ml of drink within 20 minutes after feeding, consistently gains the coveted grams, is also cheerful, sleeps and eats well, then regurgitation does not harm the body.
With age, when the baby grows up and gets stronger, the regurgitation will go away. Healthy children rarely burp after one year.
How to distinguish vomiting from regurgitation
When vomiting, a newborn spits up like a fountain, profusely. Alas, such regurgitation is not harmless; if it becomes more frequent, its volume increases, and the color and smell change. At the same time, weight gain slows down or the baby loses weight, expresses dissatisfaction with food, showing that something hurts.
Persistent vomiting, increased salivation, diarrhea, changes in general condition and development are always abnormal.
Such a baby definitely needs to be shown to a pediatrician: pathological regurgitation can be a symptom of reflux disease, food allergies, infections, diseases of the gastrointestinal tract, metabolism, nervous system, birth defect, etc.
Why does a baby spit up and what to do about it?
- Causes of spitting up in children
- What to do if your baby spits up
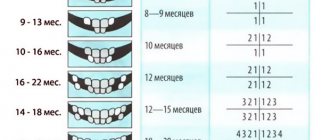
Almost all young mothers are concerned that their babies spit up after feeding. This is usually caused by aerophagia (air entering the esophagus during sucking). This is absolutely normal for infants. So, up to three or four months, 67% of infants burp, from four to seven - 21%, and even from seven months to one year, 5% of babies still sometimes regurgitate excess food.
If the child burps no more than twice a day and the volume of each regurgitation is small, then mothers have nothing to worry about - the baby’s digestion is fine. The main thing is to properly establish breastfeeding, and if the mother for some reason cannot feed the baby with her milk, select a substitute formula with the help of a doctor.