05/04/2021 897 Pulmonology
Author: Elena
In Russia, pneumonia is diagnosed in 10 young children out of 1000. Signs of pneumonia in a child depend on the age and type of the disease. Infants and children under 4 years of age are most susceptible to this pathology. Pneumonia in young children can be diagnosed using fluoroscopy. After confirming the medical report, the doctor decides to hospitalize the patient and selects antibacterial therapy. The disease lasts on average 7-10 days.
[Hide]
Types of childhood pneumonia
Depending on the location of the inflammation, pneumonia can be:
- share;
- segmental;
- right-sided;
- left-handed;
- bilateral.
Based on their form, they distinguish between community-acquired (home-acquired), hospital-acquired and congenital pneumonia. The least common is atypical childhood pneumonia caused by mycoplasma. Pneumonia, characteristic of patients with immunodeficiency conditions, is classified separately.
The most common types of pneumonia are:
- focal bronchopneumonia;
- lobar pneumonia (pneumococcal);
- segmental (polysegmental) bronchopneumonia;
- interstitial acute.
Moreover, each type of pneumonia can be divided into uncomplicated and complicated. This form sometimes entails more serious diseases, such as effusion pleurisy, lung destruction, etc.
Depending on the duration of the disease, pneumonia can be:
- acute current (lasting up to 4 weeks);
- protracted (stated when the inflammatory process in the lungs continues for more than 4 weeks).
Any untreated pneumonia, especially in children under 3 years of age, becomes chronic. This form is characterized by irreversible changes in the bronchial tree and constant relapses.
Types of childhood pneumonia
Pneumonia in adults and children: causes of inflammation
Pneumonia can occur both as an independent disease (most often viral) and as a complication after ARVI or influenza.
Infants under six months of age, as a rule, suffer from pneumonia, the causative agents of which are usually staphylococci and E. coli. This may be due to food entering the respiratory tract, which occurs due to the structure of the child’s larynx and is not normal, or due to improper care, when the child is placed on his back immediately after feeding, without turning him on his side or holding him upright. for air to escape.
Pneumococcal and hemophilic pneumonia are observed in children who have had contact with ARVI patients. As a rule, these are children from 6 months to 5 years.
Older children can suffer from pneumococcal and mycoplasma pneumonia with equal frequency.
Causes of pneumonia
Pneumonia is a complication of diseases such as bronchitis and bronchial asthma, laryngitis, pharyngitis, tonsillitis, and ARVI.
Pneumonia can be caused by:
- Viruses (diagnosed in approximately half of patients). These can be: Afanasyev-Pfeiffer bacillus, chickenpox virus, influenza, herpes, adenovirus, cytomegalovirus.
- Bacteria. Most often, pneumonia is provoked by Legionella, Escherichia, Klebsiella, and Mycoplasma.
- Fungi. The rarest and most severe form, which occurs due to improper treatment of the underlying disease, for example, after the use of antibiotics for viral infections.
- Parasites. Lung damage is caused by roundworms, pork tapeworm, and pulmonary fluke.
In newborns, pneumonia is most often caused by streptococci and staphylococci. Sometimes pneumococci and Haemophilus influenzae can be the cause.
Congenital pneumonia manifests itself during the first 72 hours of a baby’s life. Infection with bacteria and chlamydia can occur during childbirth, then neonatal pneumonia manifests itself from the 6th to the 14th day of the child’s life.
Another reason for the occurrence of the disease is the presence of intrauterine infection against the background of fragile immunity. Herpes viruses and cytomegalovirus can also be causative agents of the disease. Sometimes congenital malformations contribute to the disease.
In children older than one year, the causes of pneumonia are:
- chronic infections;
- complicated sinusitis, adenoiditis, problems of the cardiovascular and central nervous systems;
- improper treatment of acute respiratory infections and acute respiratory viral infections (in the case of the use of cough suppressants).
Frequent use of vasoconstrictor drugs, or their use when there is a strong discharge from the nose, can contribute to the descent of the virus into the bronchi.
Despite the general misconception, it is extremely rare that the cause of pneumonia is severe hypothermia in a child.
Signs of improper treatment
The first sign of improper treatment is the lack of positive dynamics. In addition, the following symptoms can be identified that indicate a violation of treatment:
- deterioration in general health;
- Worsening coughing attacks with shortness of breath, especially at night;
- severe shortness of breath that occurs even without visible effort;
- hypoxia with pale skin and blue lips;
- Airway obstruction;
- wheezing when exhaling, heard from afar;
- severe chest pain aggravated by coughing attacks;
- Discharge of large amounts of pus or blood when coughing.
Symptoms of pneumonia
The clinical picture depends on the following factors:
- forms;
- pathogen;
- degree of severity;
- child's age.
The main symptom of pneumonia is shortness of breath. A deep paroxysmal cough may occur. Possible chest cavity. If the disease is severe, the child may have attacks of suffocation during or immediately after coughing. Children's breathing quickens, becomes shallow, and it becomes impossible to take a deep breath. Pneumonia can also be recognized by wheezing in the lungs.
Additional symptoms:
- Increased body temperature, swelling of the legs.
- The face, especially the lips, turns pale or takes on a gray/bluish tint. As a rule, this is characteristic of bacterial pneumonia, and is caused by spasms of blood vessels.
- Appetite decreases or disappears completely. The child may lose significant weight.
- Lethargy, irritability, and increased fatigue appear.
In the video, the famous doctor talks about the symptoms of pneumonia. Video taken from the “Doctor Komarovsky” channel.
Signs in children of the first year of life
Pneumonia in newborns and babies in the first year of life is manifested by general lethargy and excessive drowsiness. The child refuses to eat, cries a lot, and behaves restlessly. Symptoms increase gradually. As soon as the baby’s mother notices such symptoms, you need to contact your pediatrician, even at normal body temperature. The chances of survival in young patients, especially infants, depend on the timeliness of medical care. Pneumonia in newborns, especially intrauterine pneumonia, often ends in death.
Depending on the age of the child, signs of pneumonia are:
- A one-month-old baby has respiratory failure, which occurs due to the underdevelopment of the baby’s immune system.
- In a two-month-old baby, the disease is characterized by multiple small focal lesions of the lungs.
- When three-month-old babies get sick, two lungs are affected at once.
- A one-year-old child more often develops segmental pneumonia, which can cause the most complications.
A doctor must identify the presence of pneumonia; the diagnosis is confirmed by x-rays and a blood test. The number of leukocytes, an increase in which is a sign of the development of pneumonia in children, helps to understand the presence of the disease.
First signals
The first signs of the disease in babies:
- behavioral disturbances in the direction of increased moodiness;
- frequent or loose stools;
- The cough is paroxysmal, worsens when crying, is accompanied by vomiting, yellow or green clots may be coughed up.
- the baby begins to spit up frequently between feedings;
- sleep is disturbed - it becomes intermittent, restless.
Body temperature
Body temperature in babies may remain unchanged or rise to subfibrile - 37.1-37.5 degrees. This is due to weak immunity and will not help determine the severity of the disease.
Baby's breathing
Breathing during pneumonia becomes rapid (more than 30 breaths per minute), heavy, with congestion at the site of the lung lesion. When a child gets sick, he begins to puff out his cheeks or nostrils, retract his lips and nod in time with his inhalation. Infants under 3 months of age may experience foaming at the mouth and nose, which may indicate impending respiratory arrest.
Cyanosis of the nasolabial triangle
For babies in the first year of life, blue discoloration of the nose and lips is typical. This sign can be noticed during feeding, when the baby is tense. Cyanosis can also be discernible in a relaxed state, which indicates the spread of bacteria and vasospasm.
This is what cyanosis of the nasolabial triangle looks like in a baby
Signs in preschool children
The first sign of pneumonia in children 3-5 years old is an increase in body temperature from the 3rd to the 5th day of acute respiratory viral infection.
Additional symptoms:
- Intoxication of the body increases significantly, the child becomes irritable.
- There are problems with sleep - the baby tosses and turns, wakes up, behaves restlessly, while lethargy and loss of appetite are expressed.
- Another sign of the development of pneumonia is a body temperature that is difficult to reduce. The drugs that helped before stop working.
- There is chest pain and increased sweating.
- The cough appears from the 5th day of illness or is absent.
- Sometimes skin rashes and muscle pain appear.
- Tachycardia may develop. Breathing becomes more frequent - more than 50 breaths per minute.
Signs in schoolchildren
In children 7-12 years old, symptoms are expressed as follows:
- breathing is heavy and harsh, increasing up to 60 times per minute;
- against the background of the development of pneumonia, fine wheezing appears in the lungs, muffled tones can be heard at the site of inflammation;
- body temperature rises to 39-40 degrees and lasts for 3 days, as a rule, without further increase;
- sputum does not come out well, the child suffers from a dry cough;
- pallor or blueness of the lips is noted.
What is pneumonia and how does it happen?
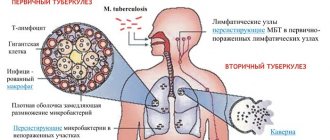
Pneumonia is an acute infectious disease of the lung tissue (parenchyma).
Experts divide it into several types.
- According to the conditions in which the infection occurred: community-acquired pneumonia and nosocomial pneumonia, pneumonia in children is divided into intrauterine and acquired.
- According to the type of causative agent of the disease - bacterial, fungal, viral.
- The severity of the disease depends on the severity of respiratory failure and intoxication.
- By nature, pneumonia without complications lasts 2-4 weeks, subacute (complicated) - up to 1-2 months and prolonged - from 1.5 to 6 months.
Segmental pneumonia
Segmental pneumonia affects entire segments of the lungs, causing them to become deformed. It can develop at any age; children aged 3-7 years are most susceptible to the disease. It is characterized by severe intoxication of the body with an increase in body temperature above 38.5 degrees. During the course of the disease, respiratory failure develops. Segmental pneumonia is treated for a long time, usually in an inpatient setting. Cough occurs rarely. Recovery of lung cells lasts for 2-3 months. Bronchiectasis may form - enlargement of individual areas.
This is what the lungs of a child with segmental pneumonia look like on an x-ray
Danger for children
The younger the child, the more atypical the disease progresses and complications are more likely to occur after pneumonia. Doctors note that pneumonia in young children is an extremely dangerous condition, since the clinical manifestations of the disease in the first days may be minimal, the body temperature is not higher than subfebrile (that is, stay within 37.1–38 ° C), and the cough is not so expressed as during the course of the disease in an adult.
Maria Organova: “More often, temperature characterizes the pathogen that caused pneumonia. With staphylococcal - it is hectic, i.e. temperature rises with rapid declines are repeated several times a day, and with mycoplasma or chlamydia it may not even rise.”
This is why experts insist on hospitalization:
- children under six months;
- children with complicated pneumonia;
- patients with dehydration and severe respiratory failure;
- children with developmental defects;
- if initial antibiotic therapy is ineffective (after 36-48 hours).
Maria Organova: “Complications after pneumonia can be of a different nature - from pleurisy, abscesses and purulent pneumothorax to death (in 5-10% of cases in the case of nosocomial infection).”
Indications for hospitalization
Newborns and children under 3 years of age must be hospitalized. Children over 3 years old are admitted to the hospital if the disease is severe or complicated by other chronic diseases. The decision to keep the child in the hospital or at home is made by the attending physician after assessing the condition of the sick baby and the results of the analysis.
Indications for hospitalization in children of primary and senior school age are lesions of several lobes of the lung, abscess or sepsis. If the pressure drops, the child faints or feels excessively weak, it is advisable to hospitalize him for constant monitoring. Any disturbance of consciousness is a reason for emergency hospitalization. At any age, children with obstructive syndrome or pleurisy are admitted to the hospital.
Treatment of pneumonia
Important: treatment should only be prescribed by a doctor. Depending on the type of disease and the nature of its course, he will determine how to treat pneumonia in a particular case and select competent antibiotic therapy for the child with the required dosage and duration of treatment. Parents must follow all doctor's instructions, since some types of antibiotics are very dangerous for children and have side effects.
In addition to treatment, the specialist may prescribe antihistamines (to exclude allergies to decay products of microorganisms against which antibiotics are used for pneumonia), vitamins, detoxification drugs, as well as general restorative therapy.
Maria Organova: “During treatment, maintain bed rest, with expansion after the temperature normalizes, do not forget to ventilate the room and humidify the air. The room temperature should be no more than 22 degrees.
Give your child plenty to drink, do not force-feed, as when the condition improves, the appetite returns on its own.”
Treatment of the disease
The principles of treating pneumonia depend on the causative agent of the disease. Viral pneumonia goes away on its own within 7 days and does not require additional treatment. Bacterial infections can only be cured with antibiotics. It is very important to provide enough fluids, even if the child refuses to drink on his own.
Standards of treatment for childhood pneumonia include the use of the following medications:
- Cough. Drugs are used to thin sputum and facilitate its removal. It can be used in the form of tablets or syrups; the composition can be chemical or natural. Well-proven ones are Ambroxol (from birth), Bromhexine (from 3 years).
- Temperature. Antipyretic medications are used if the body temperature is above 38.5 degrees. The most popular are Paracetamol (from birth) and Nurofen (from birth).
- Antibiotics. First of all, penicillin is prescribed, but the choice depends on the form of pneumonia. Popular ones are Amoxicillin (from birth), Erythromycin (from 4 months).
- Probiotics – Linex (from birth), Bificol (from 6 months).
If pneumonia occurs against the background of an acute respiratory viral infection, it is important to treat a runny nose. For swelling of the mucous membrane, be sure to use vasoconstrictor drugs - Otrivin (from 6 years), Nazivin (from 1 year). Rinse with saline solutions - Aqua Maris, Quick, Spritz, all of them can be used from birth.
For bronchial obstruction, treatment with Berodual or Eufillin is prescribed. The drugs can be used from birth under the supervision of a doctor.
The types of medications for pneumonia, dosage and method of administration are shown in the table:
| Type of medication | Drug name | Age | Dosage | Method of administration |
| Mucus thinners | Ambroxol Bromhexine | from birth from 3 years | up to 6 years – 1/2 tsp, up to 12 years – 1 tsp, over 12 years – 2 tsp. 3-6 years – 2.5 ml, 6-10 years – 5-10 ml, over 10 years – 10-20 ml | 2-3 times a day, during meals 3 times a day |
| Antipyretics | Paracetamol Nurofen | from birth from birth | 15 mg per 1 kg 50 ml | 3-4 times a day 3 times a day |
| Antibiotics | Amoxicillin Erythromycin | from birth from 4 months | 20 mg per 1 kg 50 mg per 1 kg | divided into 3 doses divided into 4 doses |
| Probiotics | Linex Bificol | from birth from 6 months | up to 7 years – 1 sachet, over 7 years – 2 sachets, up to 12 months – 1 dose, over a year – 5-10 doses | Once a day, 3 hours after the antibiotic, dissolve 1 dose in 1 tsp. water, apply 20-30 minutes before meals |
| Vasoconstrictors | Otrivin Nazivin | from 6 years from 1 year | 1 injection up to 6 years – 0.025% – 1-2 drops, over 6 years – 0.5% – 1-2 drops | 3-4 times a day 2-3 times a day |
| Wash solutions | Aqua Maris Quick | from birth from birth | 1-2 irrigations 1-2 irrigations | 3 times a day 3 times a day |
| For bronchospasm | Berodual Atrovent | from birth from birth | 2 drops (0.1 mg) per 1 kg per 1 dose, no more than 1.5 mg per day individually | inhalation through a nebulizer intravenously |
Ambroxol - 94 rubles
Amoxicillin - 101 rubles
Atrovent - 364 rubles
Linex - 536 rubles
Otrivin - 164 rubles
Paracetamol - 55 rubles
Basic rules for treating pneumonia at home
If pneumonia is diagnosed, hospital care is recommended. Treatment at home can be done with the permission of the pediatrician, provided that all instructions are followed.
The most important recommendations:
- As soon as the child begins to get sick, the temperature in his room should be 18-19 degrees, since cool air prevents the mucus in the lungs from drying out quickly.
- It is advisable to remove all dust collectors and carpets; if this is not possible, wet cleaning should be done more often. It is better to do this once a day, but at least twice a week without using detergents with fragrances.
- The room where the child is located must be regularly ventilated and moistened. To do this, you can use special household appliances, air ionizers or any other items (towels on a radiator, a bowl of water). Ventilate every 10 minutes for an hour.
How long treatment of pneumonia at home will last will depend on the child’s compliance with the drinking regime and diet. Meals should be light, without fatty and fried foods. Vegetable soups and steamed meat are ideal. If the child does not want to eat, you can limit yourself to decoctions of dried fruits, compote or tea.
The disease is treated faster if you adhere to bed rest. You can walk outside from the 6th-7th day of illness if you feel well and have favorable weather conditions.
Principles
In some cases, pulmonologists allow the child to be treated at home. The course consists of several stages and includes both antimicrobial drugs in combination with expectorants, and multivitamins to support the immune system.
General rules for treating pneumonia outside the hospital include the following:
- Using a special diet rich in vitamins and microelements, as well as completely eliminating all foods that can cause allergies;
- Avoiding contact with any allergens;
- Physical exercises (during the recovery stage);
- taking medications, including broad-spectrum antibiotics;
- folk remedies (only as an addition to general treatment).
As mentioned above, treating pneumonia at home is possible only after agreeing on all the details with the attending physician. It is extremely important to follow all recommendations of a specialist. If there is any deterioration in the overall picture or in the absence of positive dynamics, the child should be hospitalized.
Basic recommendations
Treatment at home, as in a hospital, should be comprehensive and consist of several activities simultaneously. These include:
- taking antibiotics;
- symptomatic treatment;
- diet correction;
- Exercise.
Antibiotics
Antibiotics are prescribed from the moment of diagnosis. Targeted drugs such as penicillins and antipneumococcal drugs are usually selected. At home, drugs are most often prescribed in tablets or suspensions; in hospitals, drugs are administered intravenously or intramuscularly, which in severe cases of pneumonia ensures highly effective treatment.
Symptomatic therapy
Symptomatic treatment consists of controlling cough and fever.
To normalize bronchial patency, mucolytics such as Bromhexine and Lazolvan are prescribed. To facilitate breathing and eliminate attacks of shortness of breath, doctors strictly according to indications (development of respiratory failure or deterioration of bronchial obstruction) prescribe Pulmicort and Berodual.
Massage
Massage for pneumonia is an integral part of treating the disease at home. The main purpose of the procedure is to facilitate the discharge of sputum.
The essence of the massage is rubbing the back and chest and patting movements from the lower back to the shoulders. The child should lie on a hard surface.
Additionally
A vitamin complex may also be prescribed to strengthen the immune system. The use of propolis and royal jelly also has a positive effect.
Disease prevention
Prevention is important in the treatment of pneumonia. It begins during pregnancy, when expectant mothers should avoid smoking and inhaling tobacco smoke. It is necessary to monitor your health and nutrition.
The following measures to prevent pneumonia are distinguished:
- Hardening the body. The stronger a child’s immunity, the lower the risk of developing pneumonia.
- Frequent long walks in the fresh air.
- Avoid damp, moldy or poorly ventilated areas.
- Timely treatment of acute respiratory infections and acute respiratory viral infections, especially in children of the first year of life.
In what cases is it better to go to hospital?
Is it possible to treat pneumonia at home without visiting a clinic? Treatment at home is possible only after a comprehensive examination and receipt of specialist recommendations.
Home therapy is allowed:
- at the initial stage of the disease, when changes in the lungs are minor and the child’s general well-being does not cause concern;
- If the parents are able to provide the child with proper care and timely administration of medications.
Treatment at home is prohibited in the following cases:
- If the child has severe shortness of breath;
- If there is significant damage to the lung tissue;
- In case of high body temperature;
- With the general unstable state of health of the young patient;
- if there is an increased risk of complications and a tendency to allergic reactions;
- if there is pulmonary obstruction;
- if the child develops pneumonia.
Video
In this video, a famous doctor talks about the diagnosis, prevention and treatment of pneumonia in children. Taken from the “Doctor Komarovsky” channel.
Do you have any questions? Specialists and readers of the KROHABABY website will help you ask a question
Was this article helpful?
Thank you for your opinion!
The article was useful. Please share the information with your friends.
Yes (66.67%)
No (33.33%)
X
Please write what is wrong and leave recommendations on the article
Cancel reply
Rate the benefit of the article: Rate the author ( 3 votes, average: 4.67 out of 5)
Discuss the article:
Treatment and prevention
The World Health Organization calls vaccination one of the most effective methods of preventing pneumonia: it is important to get vaccinated against pneumococcus, measles and whooping cough. In addition, it is necessary to increase the child’s body’s defenses: provide him with proper nutrition and protect him from the harmful effects of environmental factors.
“The treatment of pneumonia is always the same: it depends on the pathogen. For a bacterial infection - an antibiotic, for a fungal infection - antifungal drugs. For existing complications, such as obstructive syndrome, use mucolytic therapy if necessary. If there is no temperature, then there is no need for antipyretic drugs and nothing more. Otherwise, the treatment of pneumonia without fever is the same as with it,” says pediatrician Olesya Mukhamedyarova.
Experts emphasize: it is important for parents to be vigilant, pay attention to the slightest changes in the child’s behavior and remember that even the most serious illness is not always accompanied by a rise in temperature.
- share with your friends!
Experts: Olesya Gabdrashitovna Mukhamedyarova
How to identify and treat?
So what do the symptoms of this pathology look like? In fact, recurrent pneumonia differs little from its initial manifestation.
Newborns exhibit the following symptoms:
- persistent cough with a lot of sputum;
- heat;
- refusal to eat;
- tearfulness;
- breathing becomes deep and frequent;
- the skin turns blue.
In older children, the symptoms are slightly different:
- muffled sound in the lungs on the affected side;
- wheezing, as if from bubbles;
- dry cough with a small amount of sputum;
- temperature fluctuations that do not allow one to derive a pattern.
If all these symptoms are repeated again and again, then we can talk about recurrent pneumonia.
What is its difficulty? More severe intoxication, difficult treatment and a long recovery period (sometimes up to several months).
The most important thing to remember is that if your child gets pneumonia again, self-medication is not allowed! Relapses of pneumonia are treated only in a hospital!
A doctor can recommend treatment only after a series of detailed examinations to determine the sensitivity of pathogens to various medications.
The examination may include bronchoscopy, computed tomography of the lungs, sweat test and Mantoux test.
The second basic rule for preventing relapse of pneumonia is that a new course should not repeat the current treatment. It is customary to prescribe the latest generation of drugs to infants, since they cause minimal harm to the growing body. For example, tablets from the group of cephalosporins and fluoroquinolones.
Rule number three: immunomodulators. Since one of the reasons for the next “attack” of the disease is the child’s weak immune system, strengthening it is a top priority. Experts advise doing an immunogram, determining the state of the immune system and choosing therapy. The most commonly used are interferon or herbal preparations: lemon grass, ginseng.
You can get rid of phlegm with the help of mucolytics.
Should you stay home if your child has pneumonia?
Pneumonia is a serious disease that affects the lung tissue. Pneumonia, starting from a small segment in one of the lungs, can grow, complicating the respiratory process, affecting cardiac activity and the general condition of the body. In children, the dynamics of pneumonia are unpredictable, so diagnosis in the early stages is especially important.
Children at risk include:
- up to three years;
- premature babies, with low body weight or the presence of intrauterine pathologies;
- often ill with acute respiratory viral infections, acute respiratory infections;
- with chronic diseases, impaired blood supply, kidney and gastrointestinal tract diseases;
- from disadvantaged families living in poor living conditions;
- with moderate and severe stages of pneumonia.
The above are important criteria according to which a child is indicated for hospitalization; treatment at home will not be effective.
It is important that only a doctor can diagnose the disease; self-medication without qualified help will be a serious mistake for parents. When diagnosing pneumonia, the doctor will suggest hospitalization for the child
If parents refuse hospitalization, they must be sure that:
Having diagnosed pneumonia, the doctor will suggest hospitalization for the child. If parents refuse hospitalization, they must be sure that:
- The child’s condition will be under constant medical supervision (daily examination by a doctor at home, etc.).
- Inflammation of the lungs has not reached moderate or severe form, cardiac activity is not impaired, and there are no signs of intoxication.
- All doctor’s recommendations will be followed exactly.
- The home environment will not harm the child due to poor sanitation and hygiene.
In addition, only a child over 3, and sometimes over 5, can stay home if they have pneumonia.
Therefore, children need constant medical monitoring and care, which parents must provide at home.
Home treatment conditions
The success of home treatment of pneumonia in children depends on strict adherence to the doctor’s recommendations and compliance with sanitary and hygienic rules.
In the sequence of taking medications, you should adhere to the order specified by the doctor, especially when taking antibiotics and inhalations. Thus, taking an antibiotic should be done strictly on time, at regular intervals, and drugs for inhalation require a clear sequence.
The child should be provided with bed rest and regular ventilation of the room.During treatment, it is important to drink a large amount of liquid - water, berry fruit drinks, dried fruit compotes, tea, which will help the body eliminate harmful substances and phlegm accumulated in the lungs. The absence of fatty and spicy foods will set the body up for recovery
When treating pneumonia, do not forget about the adverse effects of antibiotics on the intestinal microflora - taking probiotics and fermented milk products will reduce the risk of dysbiosis.
What kind of illness is this?
The human lungs consist of segments - 10 in each. The segments form lobes; there are two in the left lung and three in the right. In addition to the fact that the lungs are responsible for gas exchange and saturate the body with oxygen, they are involved in a number of important processes. Therefore, with pneumonia (including latent), the entire body suffers:
- body temperature regulation is disrupted;
- neutralization and synthesis of proteins and fats worsens;
- blood is poorly cleansed;
- The body does not filter the blood well from harmful substances.
In 80% of cases, children suffer from viral and bacterial pneumonia, which is caused by streptococci and staphylococci , Klebsiella , Escherichia coli , Haemophilus influenzae , Pseudomonas aeruginosa . In rare cases, asymptomatic childhood pneumonia is caused by pathogenic fungi, and only a few cases show pneumonia due to helminths.
Asymptomatic pneumonia got its name due to its quiet course without symptoms. In infants and toddlers up to one year old, as well as in preschool children, pneumonia occurs due to pneumococci . Between the ages of 6 and 10 years, children most often suffer from mycoplasma latent pneumonia. Teenagers are most susceptible to this disease, caused by chlamydia .
Latent (sluggish, silent or asymptomatic) pneumonia is a complex form of pneumonia, the course of which is characterized by the absence of symptoms.
Asymptomatic, low-symptomatic, hidden and sluggish - in these terms we are talking about the manifestations of the disease and the severity of symptoms. And in medicine these are synonyms. “Silent” pneumonia is not a term, just as hepatitis “gentle killer” is not a term, but medical slang.
With latent pneumonia, a separate pulmonary segment or lobe becomes inflamed. The immune system gives a very weak reaction or does not respond at all to the disease. Because of this, bacterial agents multiply and produce toxins. The child suffers due to intoxication. Circulating in the blood, toxins affect internal organs.
It is difficult to notice the disease in a child, since there are no external signs, and the baby cannot point to the area causing pain and describe the deterioration of his health or the appearance of shortness of breath. Therefore, treatment often begins late, which leads to complications, such as:
- Pleurisy - fluid accumulates between the two pulmonary membranes.
- Pulmonary destruction - lung tissue is destroyed.
- Cardiopulmonary failure - blood circulation is impaired because the body does not have enough oxygen.
Be careful! These diseases in children often lead to death. To protect your child, you must take all measures to prevent complications.
Symptoms of inflammation in children over two years of age
More often, pneumonia develops in the presence of a cold. And a sharp jump in temperature during the improvement stage should worry parents. During the same period, intoxication symptoms and cough may increase.
The child may experience prolonged, up to a week, lethargy and sleep disturbances. Shortness of breath appears, breathing becomes more frequent. Possible pale skin. A high temperature that lasts longer than 4 days and is not brought down by traditional means can also signal the presence of an inflammatory process in the lungs.
Methods for diagnosing the disease in children
The primary method for identifying the disease is an initial appointment, which includes a survey, listening with a stethoscope, measuring body temperature, examination and palpation (palpation). If certain symptoms are present, the patient is sent to confirm the diagnosis - an x-ray examination. The image will indicate the exact location of the affected source of infection. This information is especially important for repeated cases of pneumonia.
To identify the type of pathogen, a laboratory test of mucous discharge from the nose and sputum is prescribed. For these purposes, the following methods are used:
- immunoenzyme;
- immunofluorescent;
- DNA polymerase.
A general blood test shows the number of leukocytes, acceleration of ESR and toxic granularity of neutrophils.
The role of antiviral therapy in pneumonia
It is known that inflammation of the respiratory tract is usually a complication caused by a viral or bacterial infection. Even an experienced doctor cannot determine whether pneumonia is viral or of another nature and make a final diagnosis regarding the cause of the disease during the first examination of a small patient. To do this, it is necessary to do a number of clinical and laboratory tests, for example, conduct a sputum, blood test, and take an X-ray of the lungs. All this takes time, which, as a rule, is not much. Therefore, most often the doctor is prompted to the viral nature of pneumonia by a characteristic sound when listening to the respiratory tract. Thus, doctors can rightfully prescribe antiviral drugs. Such drugs include Viferon Suppositories. It contains interferon protein, which prevents the proliferation of viruses, as well as vitamins C and E, which are antioxidants and contribute to the better functioning of interferon in the human body. Thanks to its dosage form (rectal suppositories), Viferon, when introduced into the patient’s rectum, begins to act very quickly, without creating additional stress on the baby’s digestive system. The drug is indicated for children from the first days of life, and even for premature babies. The use of the drug VIFERON® as part of complex therapy makes it possible to reduce therapeutic doses of antibacterial and hormonal drugs, as well as reduce the toxic effects of this therapy.
Hilar pneumonia: signs and special properties
This form of the disease differs in the location of the infection - it affects tissue at the pulmonary root, so hilar pneumonia is very difficult to diagnose. Different studies - x-ray, inspection and listening - can provide different information about the location of the lesion. If this happens, then most likely the child has basal pneumonia.
The disease is protracted; it may occur with pronounced symptoms of intoxication, but it may also not have them. Often it occurs without breathing problems or wheezing, with only a slight increase in body temperature. The presence or absence of symptoms depends primarily on the type of pathogen.
In infants, the presence of the disease can be determined if the baby often asks for the breast, but sucks sluggishly, the nasolabial triangle takes on a bluish color, and the skin in the intercostal space is retracted when breathing. If signs are present, they manifest themselves in the following conditions:
- severe, paroxysmal dry cough;
- release of large amounts of sputum;
- hard breathing;
- wheezing;
- rhinitis;
- sore throat;
- weakness and chills at the very beginning of the disease.