I simply cannot stay away from the heated debate on the Internet regarding an important question for expectant parents: should a newborn be given a painful injection of vitamin K while still in the hospital? Is it worth exposing a child to such a test once again? Is there a more humane alternative? After all, the future happy childhood of the baby depends on their correct decision. There is a lot of information on the Internet and it is all contradictory. I will try to touch on all aspects regarding vitamin K and offer a very friendly solution that will not injure the child.
Why is a vitamin K injection given immediately after birth?
Vitamin K is necessary for normal blood clotting in children and adults. Some children (more and more of them lately) are born with low levels of this vitamin, due to the immaturity of the liver and gastrointestinal tract, where vitamin K is synthesized. In utero, the baby cannot receive vitamin K because it is not absorbed through the placenta. Breast milk contains very little of it. This condition can cause bleeding called hemorrhagic disease of the newborn (HDN). Internal bleeding in the brain and other organs can cause serious damage, sometimes even death.
Despite the fact that this disease is rare (the causes and what percentage are indicated below), vitamin K is administered intramuscularly to everyone as a preventive measure, the basis is protocol No. 152 of 04/04/2005 for a medical examination of a healthy newborn child (https://sop.com .ua/regulations/2340/2592/2593/420061/), changes since 2010, paragraph 10.
Possible side effects
After intramuscular administration of drugs to replenish the element, undesirable reactions are possible. Therefore, medications are used strictly as prescribed by the doctor, under constant monitoring of the newborn’s condition and monitoring of laboratory parameters.
Allergy
The reaction manifests itself in the form of redness of the skin and rash, urticaria. The lesion is the injection site and can be observed on the face.
Bronchial spasm
Bronchospasm is a consequence of intramuscular administration of Vikasol and other forms of vitamin K, which reduces the lumen of small bronchi and bronchioles and causes heavy breathing and shortness of breath, which are life-threatening.
Increased toxicity
Vikasol, when used together with drugs that affect hemolysis, can lead to frequent adverse reactions.
Hemolytic anemia
With this pathology of the circulatory system, a significant part of the red blood cells fades away, resulting in general swelling of the baby, jaundice, enlargement of the liver and spleen, bruising and pale skin.
Increased heart rate
Tachycardia and “weak” pulse filling can also be a consequence of injections.
Three forms of vitamin K
There is a large group of forms of vitamin K that are similar in their chemical composition and effect on the body (from vitamin K1 to K7). The most interesting of them are the two main forms that exist in nature: vitamin K1 and K2 .
Vitamin K1 (phylloquinone and its isomers: phytomenadione, phytonadione) - occurs naturally in plants, especially green leafy vegetables, which are the main pharmaceutical raw materials for the production of isomers. Only the natural form of vitamin K is completely SAFE for newborns and does not cause toxicity even in large dosages! How it works: it targets the liver, participates in the production of proteins that regulate blood clotting and thrombus formation.
Vitamin K2 (menaquinone) is a substance that is synthesized in the human body by microorganisms (saprophytic bacteria) in the small intestine. How it works: It affects the walls of blood vessels and bones more than the liver tissue. Its main task is the correct distribution of calcium in the body.
Vitamin K3 (menadione) is a synthetic form that is clearly toxic, interfering with the function of glutathione, a natural antioxidant in the body, resulting in damage to cell membranes, especially over time. Menadione also causes toxic reactions in liver cells, weakens the immune system, causes abnormal red blood disorder, and also leads to cytotoxicity (cell death). It is important to note that there was toxicity in infants injected with this synthetic vitamin K3. Widely used in the food industry and livestock farming.
Forms
Vitamin K comes in three forms, differing in properties and level of toxicity.
Phylloquinone
It is otherwise called vitamin K1. The source of the element is green leaves of plants (spinach, parsley), and some other foods. Therefore, this substance enters the body mainly with food. Isomers of the element are produced by pharmaceutical companies from natural, natural raw materials.
Menaquinone
Vitamin K2, or menaquinone, is a compound synthesized in the human small intestine. However, the substance was not found in newborns, since the intestines are not populated with the necessary bacteria during breastfeeding or are sterile during cesarean section or premature birth.
Menadion
This form of the vitamin is synthesized industrially and, when used in the human body, is converted from K3 to K2 (menaquinone). Drugs containing this substance are unsafe for a newborn due to deterioration of the liver and immune system, suppression of the function of protection against free radicals, and the functioning of the hematopoietic system may be disrupted.
There are three types of vitamin K deficiency
Early HDN occurs within 24 hours of birth.
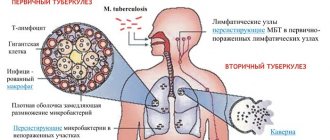
It occurs almost exclusively in infants of mothers taking drugs that inhibit vitamin K, such as anticonvulsants (carbamazepine, phenytoin and barbiturates), antituberculosis drugs (isoniazid, rifampicin), some antibiotics (cephalosporins) and vitamin K antagonists (coumarin, warfarin). The clinical picture is severe: head hematoma, intracranial and intra-abdominal hemorrhage. The incidence in newborns without vitamin K supplementation varies from 6% to 12% .
Classic HDN occurs between the 1st and 7th days of life.
Associated with delayed or insufficient nutrition. Clinical manifestations are mild: skin bruises, bleeding in mucosal tissue (mouth, nose, throat, intestines, uterus, urethra), bleeding from the umbilical cord or circumcision site. However, blood loss can be significant, and intracranial bleeding, although rare, does occur. Frequencies range from 0.25% to 1.5% in older reviews 19 and 0–0.44% in more recent ones.
Late TTH occurs between 2 and 12 weeks.
Most cases occur between 3 and 8 weeks of age. Associated exclusively with breastfeeding. The clinical picture is severe: mortality is 20%, and intracranial bleeding is 50%. Survivors suffer permanent neurological damage. The incidence in fully breastfed infants who did not receive vitamin K at birth is 1/15,000 to 1/20,000 . Children with cholestasis syndrome are at particular risk.
(Source 1, Source 2)
Types of vitamin K deficiency in newborns
Lack of vitamin K in newborns is dangerous for the occurrence of hemorrhagic disease. Against the background of insufficiency, the synthesis of blood coagulation factors is disrupted:
- prothrombin;
- proconvertina;
- antihemophilic globulin B;
- prothrombinase, Stewart-Powell factor.
Vitamin K deficiency in newborns provokes increased bleeding, which can lead to hemorrhages in various organs.
There are three types of hemorrhagic disease. The timing of symptoms varies.
Early type
Acute vitamin K deficiency in newborns, which manifests itself in the first 12-36 hours after birth, is classified as the early type. This species is not common. Most often it is a consequence of the mother taking various medications during pregnancy. It begins with the appearance of the following symptoms:
- petechial rash - small hemorrhages under the skin that can occur in the prenatal period;
- ecchymoses, or bruises;
- internal bleeding into the liver, adrenal glands, spleen and lungs;
- the appearance of intrauterine cerebral hemorrhage;
- vomiting like “coffee grounds” with blood.
Classic type
This type of vitamin K deficiency in newborns is the most common. It is observed from the second to the sixth day after birth, most often on the 4th day. It is associated with breastfeeding problems in the form of delayed early attachment to the breast. Manifested by symptoms:
- black chair;
- bleeding from the umbilical wound;
- cephalohematomas - hemorrhage between the periosteum and the outer surface of the skull;
- subcutaneous hematomas;
- intracranial hemorrhage;
- gastrointestinal bleeding, which is accompanied by jaundice;
- erosion of the mucous membranes of the duodenum.
Late type
This type of pathology develops after the first week of life. It can appear up to 4 months. Occurs against the background of concomitant diseases and in the absence of prevention. It's going hard. Mortality occurs in 20%. The brain is the first to suffer. Intracranial bleeding occurs. Hemorrhagic shock is possible. Even with effective treatment, neurological changes remain for a long time.
Hemorrhagic disease is treated in an inpatient setting. Injections of vitamin K are performed. In difficult cases, intravenous infusion is used. Newborns are treated with Vicasol, a synthetic vitamin K. Transfusions of saline and 10% glucose solution are used as anti-shock therapy. Plasma transfusion is effective. In addition to plasma, hemorrhagic disease is treated with infusion of prothrombin complex and a mixture consisting of thrombin, aminocaproic acid and adroxon.
Increased risk factors for tension headaches
Even any point is sufficient for the risk of bleeding in an infant:
- premature babies, low birth weight
- delivery using forceps or vacuum extraction
- caesarean section (the baby's microflora remains sterile after such a birth)
- very fast or long labor, especially in the second stage of labor (expulsion of the fetus)
- maternal intake of antibiotics, anticoagulants, anticonvulsants during pregnancy, especially in the first trimester
- undetected liver disease, stress on the liver after hepatitis B vaccination
- administering medications to a newborn for any reason
Data taken from an article by Dr. Joseph Mercola, USA - https://1796web.com/vaccines/opinions/vitamin_k.htm, but most of the information is out of date at the moment.
I would like to add some additional information based on new facts about the risk factors for late TTH: Bleeding due to vitamin K deficiency can happen to any child, whether early or long-term, trauma or no trauma. Researchers have not been able to pinpoint which children are most at risk. This is why doses of vitamin K are prescribed to all newborns or those whose mothers intend to breastfeed exclusively.
In fact, there is no recent evidence to support the theory that babies born by forceps or by Caesarean are at higher risk of bleeding.
One of the largest 2013 studies on the topic in Southeast Asia followed Thai women during pregnancy and after birth and examined risk factors for vitamin K deficiency. The researchers labeled infants as "high risk" for vitamin K deficiency if they had small for gestational age, born prematurely, or born by cesarean section or vacuum delivery. The researchers found no difference in the percentage of infants with vitamin K deficiency between low- and high-risk infants.
Regarding insufficient breastfeeding in the first hours of life, there is an association between insufficient breast milk in the first few days of life and classic TTH. And it is theoretically possible that a traumatic experience at birth will cause a baby to bleed more often during the first week of life if they have low vitamin K levels. But the study (see above) did not support the theory that traumatic deliveries are directly linked to vitamin K deficiencies.
Thus, the most important risk factors for TTH are exclusive breastfeeding and avoidance of vitamin K. Evidence does not support the theory that trauma at birth has anything to do with TTH.
Deficiency Prevention Measures
There are no ways to prevent vitamin K deficiency in newborns, since the causes of deficiency and complications have not been fully identified.
The main recommendations are aimed at the relationship between the pregnant woman and the treating gynecologist and therapist:
- timely observation and registration;
- if possible, do not take prohibited drugs that lead to deficiency - anticonvulsants, antibiotics, anticoagulants, or choose the safest and most studied groups;
- following the recommendations of specialists, undergoing ultrasound and screenings;
- During childbirth, interaction with a midwife and gynecological surgeon.
Currently, doctors are less likely to use obstetric forceps due to their unsafety. During prolonged labor, labor is most often stimulated, and certain risks and dangers for mother and child are weighed.
In Europe, vitamin K injections to newborns in the maternity hospital are given in 100% of cases to prevent hemorrhagic disease. In Russia and other countries, a neonatologist assesses the baby’s condition and risk factors and acts according to the protocol. To reduce the side effects of the drugs used, correct dosage calculation and careful observation, blood sampling to monitor laboratory parameters are necessary.
Side effects from the injection that you are not warned about
There are four main areas of risk associated with this injection:
- A study published in 2004 found that very early pain or stressful experiences have long-term adverse effects in newborns, including changes in the central nervous system and changes in the sensitivity of the neuroendocrine and immune systems into adulthood. A defenseless and innocent baby will have to overcome emotional trauma to achieve health.
- The amount of vitamin K given to newborns is much higher than the recommended daily dose for adults. In recent years, the situation has begun to change for the better; in any case, you should consult your pediatrician about the dose that is suitable for your child.
- An injection for a baby’s weak and immature immune system creates an additional risk of introducing infection from the environment, which contains dangerous infectious agents. As well as irritation of the injection site or damage to nerves and muscles, since the injection is made deep into the muscle. This is a rare complication, but still.
- The injection solution contains preservatives that are toxic to the baby's immature immune system. There are currently 2 forms of vitamin K used for injection: Kanavit, Konakion (K1 as phytomenadione) and a cheaper option - Vikasol (K3 as menadione, menadione). Both are synthetic forms, the latter is even more active and stronger.
Vikasol gives a lot of side effects, even if you do not consider the preservatives in the composition: facial hyperemia, itching, bronchospasm, hemolytic anemia, cytotoxicity of liver cells leading to jaundice, tachycardia. Our official medicine does not confirm this. For these reasons, the US has banned the use of synthetic K3 to treat vitamin K deficiency.Kanavit, Konakion was developed and approved for use solely on the basis that it appears to cause less hemolysis. It is a synthetic petrochemical derived from 2-methyl-1,4-naphthaquinone in a polyethoxylated castor oil or polysorbate-80 base. Although these drugs are easier to tolerate, in the annotations we see the following adverse reactions: skin rash, burning pain and inflammation at the injection site, cardiovascular collapse, bronchospasm, problems with the gastrointestinal tract.
There was also a reported case in 2014 of anaphylactic shock due to intramuscular administration of vitamin K1 in a newborn.
The poor mother has to make a choice and purchase one drug or another. As far as I know, it is difficult to get Kanavit or Konakion in Russia; they do not produce it or import it.
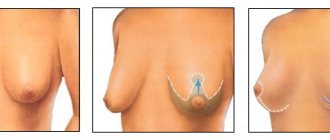
How and when injections are performed
A simple way to deliver vitamin K is by intramuscular injection of the appropriate drug. A vitamin K injection is given to the front of the thigh. Injection of the drug is carried out over several weeks or until the newborn baby’s body is mature enough to independently produce the biologically active component.
If some parents do not want to burden their child with injections, then they are offered to administer the drug orally. From an efficiency point of view, this method is not preferable. In addition, in clinical practice there have been cases in which oral use of vitamin K caused vomiting in a newborn. The standard injection plan for this substance is as follows:
- The first injection is performed immediately after birth;
- The second injection is given one week later;
- The 3rd injection is performed 1 month after the birth of the baby.
Important! Both parents and doctors should not forget that the oral use of vitamin K preparations is strictly contraindicated in children born before the expected term. A similar ban applies to children who have congenital diseases.
For injection administration to a newborn baby, analogs of vitamin K are used - Vikasol and Kanavit.
The few side effects that occur in newborns when these medications are administered are associated with the preservatives used in the manufacture of medications. Subscribe to our VKontakte group
A simple solution that replaces a vitamin K injection
According to the world's best expert on vitamin K - Associate Professor of the Department of Biochemistry at the University of Maastricht (Netherlands) Dr. S. Vermeer, there are safer and non-invasive (that do not disturb the natural integument) ways to replenish the level of vitamin K in a newborn that do not have dangerous consequences. We are talking about oral intake of natural vitamin K, which eliminates overdose and reduces the risk of bleeding and jaundice, as well as pain at the injection site and exposure to harmful preservatives. At the same time, vitamin K is absorbed through the intestines, as it is intended.
Is it really that simple, I suggest you dig deeper and turn to official sources...
Oral Vitamin K is a Safe and Effective Alternative
Fortunately, while recent research has shown that there are safer and better methods that will be just as effective in protecting your child from TTH, the alternative to this blatantly unnecessary injection is surprisingly simple: give the vitamin orally. It is safe and equally effective, and free of the previously mentioned worrying side effects.
Orally administered vitamin K is absorbed less efficiently than parenterally administered vitamin K. However, this can be easily corrected by adjusting the dose. And since vitamin K is non-toxic, there is no danger of overdose or adverse reactions.
The Science behind Oral Vitamin K vs Injectable Vitamin K
Recent studies show:
- the chance of late TTH is 1 in every 15,000-20,000 children when vitamin K is not given,
- if an infant has one oral dose of vitamin K (1-2 milligrams) at birth, the risk drops to 1 in 25,000-70,000 children,
- The odds of late-onset HDN in a newborn are reduced to 0.1 per 100,000 children when the child is given 1.0 mg of synthetic K1 at birth.
In 2003, Swiss surveillance adapted recommendations for preventing vitamin K deficiency following a 6-year follow-up : “3 2 mg oral doses of vitamin K1 adequately prevent children from all types of HDN. The main risk factors for HDN in infants are parental refusal of Vitamin K prophylaxis or unrecognized cholestasis due to biliary atresia in the baby.”
In 2008, a comparative analysis of the effectiveness of various vitamin K administration regimens among infants with biliary atresia was carried out in Holland and Denmark : “A daily dose of 25 mcg of vitamin K does not prevent bleeding, but 1 mg weekly oral prophylaxis provides significantly higher protection for these infants and has similar efficacy as 2 mg intramuscular prophylaxis at birth."
And a more recent study in 2021 did not support the effectiveness of oral regimens versus the injection in infants with cholestasis.
A 2006 study of preterm infants reported an interesting finding: “To protect against bleeding due to vitamin K1 deficiency, preterm infants receiving a 0.2 mg dose intramuscularly should receive vitamin K supplementation during breastfeeding.”
What are the benefits of vitamin K injection?
- Very effective in preventing classic and late-onset TTH
- The shot has a slow-release effect over time from the injection site, which provides sufficient amounts of vitamin K1 until levels in the child's blood reach completely natural levels.
What are the benefits of oral vitamin K?
- Easy to give, non-invasive, no harmful substances in the composition
- The 3-dose regimen reduces the risk of classic and late-onset TTH, but not as much as the injection
- A weekly regimen appears to protect children with undiagnosed gallbladder problems as much as the shot
Conclusions: The effectiveness of oral prophylaxis is related to the dose and frequency of administration. Most multidose oral regimens provide protection for all but a small number of infants with gallbladder or liver disease. However, looking specifically at vitamin K levels, it was found that a vitamin K shot resulted in elevated blood levels over one week and one month compared to a single oral dose. And in all this time, none of the studies specifically looked at whether there were any side effects from the injection.
An alternative to injections is oral administration.
Since the development of drops that can replace painful injections, many studies have been conducted looking at how effective vitamin K drops are for newborns.
- A study conducted in Denmark and Holland in 2008 found that oral and intramuscular administration were equally effective in children diagnosed with biliary atresia.
- Data for 2021 revealed a low effect of oral administration of the drug in children with cholestasis.
- The Swiss Epidemiological Service conducted observations for six years and, as a result, created recommendations for ingesting drops: three times.
Using drops has certain advantages:
- does not cause pain to the baby;
- parents can give them at home;
- reduces the risk of hemorrhagic disease in healthy infants.
Disadvantages of drops:
- the need for repeated administration during regurgitation;
- low performance for children at risk;
- duration of admission.
Drops should be given to children only after meals, and the dosage must be observed.
Which Vitamin K1 drops to use and what dosage
Many scientific articles state that oral vitamin K1 is not available in the United States. This is because there is no FDA-approved oral version available for sale. However, all English-language sources for purchasing high-quality vitamin K1 in drops lead to Bio-K-Mulsion from the American manufacturer Biotics Research .
It contains another isomer of phylloquinone, phytonadione , created in the laboratory from naturally occurring bacteria. Of course, it is also synthetic, like Kanavit, but it is much safer to take orally than by injection, and has the advantage that few drops are required per dose. Natural K1 drops require 40 to 150 drops to achieve a similar dosage. This may not be appropriate for an infant.
And where can you buy the liquid oral form of vitamin K1? Unfortunately, my favorite store iherb did not have vitamin K1. You can just as easily make a purchase on Amazon; at the end of the post I will talk about two more important related products needed after childbirth.
Biotics Research - Bio-K-Mulsion 1oz, 30 ml
Active Ingredients: Vitamin K (as K1-phytonadione) This is a manufactured form of vit k1 as the real form is unstable and too strong. This product is made from naturally occurring bacteria to achieve a stable and beneficial form.
Four drops (0.16 ml) provide 2 mg of vitamin K1. Bio-K-Mulsion® delivers Vitamin K1 (500 mcg per drop) in emulsified liquid form to aid in the absorption and utilization of this important vitamin. Vitamin K oil has been dispersed into microscopic particles to promote better absorption.
Other Ingredients: Water, gum arabic oil and sesame oil.
Dosage regimen: 2 mg (4 drops) within 6 hours after birth, on the 7th day of life - 1 mg (2 drops) and then weekly for the first 3 months of life. If the child burps within 1 hour of oral administration, this dose should be repeated.
If the seller has run out of Bio-K-Mulsion, there is still a good option from a highly rated American manufacturer - Herb-Science
Herb-Science, Liquid Vitamin K1 Drops, 1 Fluid oz, Alcohol Free
Active Ingredients: Vitamin K (as K1-phylloquinone) Serving Size: 1 dropper (0.8 ml) contains 120 mcg of liquid vitamin K1 Cold processed to protect compounds. Contains no alcohol, sugar, salt, yeast, wheat, gluten, corn, soy, milk, egg, shellfish and no artificial preservatives. Other Ingredients: Safflower Oil.
Dosage regimen: 2 mg (16 pipettes is 13 ml) within 6 hours after birth, on the 7th day of life - 1 mg (8 pipettes is 6.4 ml) and then weekly for the first 3 months of life. If the child burps within 1 hour of oral administration, this dose should be repeated.
It is important to remember that this fat-soluble vitamin cannot be absorbed on an empty stomach . Therefore, it is given before or after breastfeeding and care is taken to ensure that the baby does not burp.
Many mothers have got the hang of it: they put a drop of vitamin K on their finger and squeeze out fatty colostrum there and let the baby suck, and so on 4 times :)).
One of the difficulties of taking vitamin K this way is maintaining the dosage schedule for 3 months. Although you can set a reminder on your smartphone. The fact is that repeated doses reduce the further risk of developing late HDN, which can occur even in completely healthy children during an ideal birth.
Overdose
Phytomenadione has low toxicity, and its overdose does not cause clinical problems. Internal administration of a drug containing phytomenadione can cause acute hypersensitivity or an anaphylactic reaction, which is manifested by hot flashes, sweating, chest pain, difficult breathing, cyanosis, bronchial constriction and cardiac-vascular collapse. These reactions are likely to be caused by histamine-induced effects due to other substances, not to mention the medicinal substance.
In newborns, especially premature babies, a high dose can lead to hemolytic anemia. There is also a risk of nuclear toxicity caused by the depletion of bilirubin in the bonds with albumin.
Treatment: in case of overdose, treatment is not required, since there are no serious clinical symptoms, since the biological period of phytomenadione is short (from 1.2 to 3.5 years).
What prevention strategy should you choose for your child?
Of course this is a very difficult choice. My goal was to provide more information so that you can draw your own conclusions and evaluate the risks of different routes of vitamin K administration.
The table at the bottom of this post contains approved preventive methods from different countries.
The intramuscular route of administration of vitamin K has been widely accepted as it virtually eliminates the possibility of life-threatening tension-type headache. At the same time, the Italian Society of Neonatology recommends taking oral drops after the injection to prevent late bleeding, especially in premature infants.
In any case, in all countries except the United States, parents have the right to refuse the injection and document oral vitamin K intake by notifying their birth team. The Danish regimen of 2 mg oral vitamin K after birth and 1 mg weekly appears to protect children at increased risk who have undiagnosed gallbladder disease, but not 100%. It is important to adhere to all weekly doses to ensure this regimen helps reduce the risk of late-onset TTH.
Using the same source, I would like to draw your attention to the facts for which it is simply necessary to use a vitamin K injection:
- Once the diagnosis of HDN has been confirmed, intravenous administration is advisable, determined by the doctor;
- Premature newborns will not physically be able to “digest” oral medications;
- Infants of mothers taking medications that inhibit vitamin K
Lately, there have been a lot of myths, misconceptions and misinformation spreading across the internet and social media about vitamin K. It is important that parents look at the facts before making such an important decision.