What is hydrocele?
Hydrocele, also known as hydrocele or hydrocele, is an accumulation of fluid in the membranes of the testicle, which leads to enlargement of the scrotum, and sometimes swelling in the groin area.
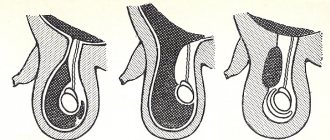
There is isolated hydrocele of the testicular membranes, when the fluid surrounds the testicle and cannot flow into other cavities, and communicating hydrocele.
A communicating hydrocele differs in that hydrocele can flow into the abdominal cavity and back through a special duct - the vaginal process of the peritoneum. Hydrocele of the testicle is often combined with an inguinal hernia.
Lymphocele is a concept close to testicular hydrocele, meaning the accumulation of lymph in the membranes of the testicle, which occurs when the lymphatic vessels of the testicle are damaged or compressed. Typically, lymphocele is accompanied by stagnation of lymph in the testicle and its membranes - lymphostasis.
Classification of the disease
Hydrocele can be isolated or communicating:
- Communicating hydrocele is a congenital type of pathology and is observed in newborns. It is characterized by the presence of a duct between the abdominal cavity and the scrotum. In this case, there is free circulation of peritoneal fluid and its accumulation in large quantities in the scrotum. Such dropsy can become isolated.
- Isolated - peritoneal fluid is not formed in the abdominal cavity, but directly in the scrotum. Most often the disease is one-sided.
The disease is divided into congenital and acquired. The congenital form up to 1-1.5 years is considered physiological and often goes away on its own without medical intervention. Acquired dropsy is the result of injury, previous infections, etc.
According to the mechanism of development, primary and secondary hydrocele are distinguished. The primary is related to the anatomical features of the boy’s body. Secondary dropsy occurs due to another disease, condition, or injury.
Communicating hydrocele of the testicle in children. What is the mechanism of formation of a communicating hydrocele?
The term communicating hydrocele or communicating hydrocele means that between the cavity surrounding the testicle and the abdominal cavity there is a communication - an open vaginal process of the peritoneum, through which fluid from the abdominal cavity enters the scrotum and back.
During fetal development, the testicle descends into the scrotum through the inguinal canal. Together with it, the processus vaginalis descends into the scrotum - an outgrowth of the peritoneum that envelops the testicle and, thus, forms the two shells closest to the testicle.
By the time of birth or during the first months of life, normally the processus vaginalis of the peritoneum is overgrown, and the connection between the testicular membrane and the abdominal cavity disappears. Thus, neither peritoneal fluid nor abdominal organs can penetrate the cavity where the testicle is located. The lower part of the processus vaginalis of the peritoneum forms a slit-like cavity around the testicle, which, in case of dropsy, serves as a container for dropsy fluid.
The main cause of communicating hydrocele of the testicle is non-closure of the processus vaginalis of the peritoneum, which serves as a duct for moving peritoneal fluid from the abdominal cavity into the membranes of the testicle.
Causes of non-fusion of the peritoneal process.
Many theories explain non-fusion of the processus vaginalis of the peritoneum. Thus, in the open vaginal process of the peritoneum, smooth muscle fibers were found, which are not found in the normal peritoneum. Smooth muscles can prevent fusion of the peritoneal process.
According to our data, there is a higher incidence of reported hydrocele in children born after a pathological pregnancy with threatened miscarriage, as well as in premature children.
Another reason lies in the increase in intra-abdominal pressure, which is observed during resuscitation measures, with frequent restlessness of the child or during physical exercise.
Causes of the disease
Acquired dropsy:
- injury;
- tumor;
- inflammation;
- complication of various diseases;
- previous infection;
- severe vascular and heart diseases;
- the result of unsuccessful surgery;
- performing peritoneal dialysis;
- testicular torsion;
- disturbances in the functioning of the lymphatic system, resulting in the formation of excess lymph that accumulates in the membranes of the testicles.
Congenital hydrocele:
- birth injury;
- pathologies during pregnancy;
- prematurity;
- developmental anomalies in infants;
- infection suffered by the expectant mother during pregnancy;
- abdominal wall defects;
- risk of miscarriage;
- location of the testicles outside the scrotum;
- hypospadias (penis malformation);
- non-fusion of the vaginal process.
Causes of isolated dropsy:
- Anomalies in the fusion of the inner membrane of the testicles. Normally, it should turn into connective tissue that cannot produce fluid. If the fusion occurs incorrectly, then the gap between the abdominal cavity and the scrotum disappears. However, the inner lining of the testicle can produce fluid, just like the peritoneum. The fluid cannot drain into the abdominal cavity and accumulates in the scrotum.
Causes of communicating hydrocele:
- An anatomical feature of the development of the scrotum, in which the canal between the abdominal cavity and the scrotum does not heal. As a result, fluid circulates into the scrotum.
Primary hydrocele appears without concomitant pathology and is the result of structural features of the body. Secondary dropsy develops due to infection, injury, disruption of the processes of reabsorption and filtration of fluid produced by the vaginal membrane. Such pathologies are usually caused by testicular torsion, tumors of the appendages and testicles, complications of influenza, ARVI, mumps, and surgery for a hernia.
The appearance of dropsy is promoted by increased intra-abdominal pressure. In early childhood, it occurs against the background of colic, constipation, and crying. In older boys - when lifting heavy objects, physical activity, severe coughing, straining during bowel movements.
What does communicating hydrocele of the testicular membranes and an inguinal hernia have in common?
An inguinal or inguinal-scrotal hernia occurs in children with a wide, unclosed processus vaginalis of the peritoneum. Not only fluid from the abdominal cavity penetrates into the open vaginal process of the peritoneum, but also movable organs of the abdominal cavity (loop of intestine, strand of omentum, appendages in girls, etc.) can emerge, which characterizes an “oblique” inguinal or inguinoscrotal hernia.
In adults, inguinal hernias differ from those in children. They are associated with defects in the muscles and tendons of the anterior abdominal wall that occur during exercise. In childhood, such hernias are extremely rare. Therefore, operations for inguinal hernias in children and adults are performed using various methods.
Complications of dropsy
Infertility. Impaired spermatogenesis - one of the most common causes of infertility can be a consequence of impaired blood microcirculation and temperature due to the pressure of excess fluid in the testicles.
Hernias (inguinal or inguinoscrotal). With a communicating form of dropsy, the unclosed lumen of the vaginal process of the peritoneum can gradually increase and turn into a hernia.
Pain syndrome. Pain, which can become a serious psychological problem for a child, is uncommon with dropsy. The exception is acute hydrocele with a significant increase in testicular volume.
Hydrocele of the testicular membranes in newborns and young children. Isolated hydrocele of the testicle.
In newborns and infants, hydrocele of the testicle in 80% of cases is (or becomes during the first months of life) isolated from the abdominal cavity and goes away on its own within 6-12 months. Isolated hydrocele of newborns is associated with birth trauma, peculiarities of hormonal status and the state of lymph outflow from the scrotum in children 1 year of age.
Isolated testicular hydrocele is often bilateral. Often the dropsy increases and becomes tense. In cases of intense hydrops, punctures are usually performed to remove fluid from the membranes of the testicles. Surgical treatment is usually not indicated.
Isolated hydrocele of the testicular membranes in boys over 3 years of age.
Isolated hydrocele of the testicle over the age of three often occurs after injury or inflammation. There are also cases of transformation of a communicating dropsy into a non-communicating one, due to the closure of the lumen of the peritoneal process from the inside, for example, by a strand of the omentum.
Symptoms
With hydrocele in boys, the scrotum increases in size on one or both sides. In the case of a communicating hydrocele, the enlargement of the scrotum is transient; in isolated cases, the scrotum enlarges gradually. The size of the scrotum in boys with hydrocele can reach the size of a goose egg, and in advanced cases, a child’s head. Communicating hydrocele in boys can have different sizes and tensions during the day: the swelling of the scrotum reaches its greatest size during the day, when the child moves; at night, in a lying position, the tumor may disappear due to the emptying of the contents of the hydrocele into the abdominal cavity. Hydrocele in boys, as a rule, is painless and without signs of inflammation. With secondary infection of the hydrocele, pain, redness of the scrotum, chills, fever, and vomiting may occur. With a large volume of accumulated fluid, children may have difficulty urinating and develop acute urinary retention. Older children report unpleasant bursting sensations, heaviness in the groin area and discomfort when walking.
How common is testicular hydrocele and how often is surgery required?
Hydrocele of the testicular membranes in newborns and boys in the first year of life occurs in 8-10% of cases. In 80% of cases it is isolated and goes away on its own. In 20% of children, surgery is performed after one year.
Communicating hydrocele of the testicle in children after 1 year 0.5-2.0%. In 95% of cases, surgical treatment is indicated.
Lymphocele and testicular lymphostasis in adolescents after operations for varicocele account for from 1% to 25% of all surgical interventions, depending on the type of operation and surgical technique (on average about 10-12%). In 80% it is amenable to conservative treatment. In the remaining 20%, surgical treatment is indicated.
Hydrocele and lymphocele after surgery for inguinal hernia in adolescents - statistics are the same as in adults 3-10%. Surgical treatment is often performed.
How to diagnose hydrocele?
The disease usually occurs with obvious external manifestations - swelling (increase in volume) of the scrotum on one or both sides. Scrotal enlargement may decrease or disappear at night when the child is in a horizontal position, and reappear when awake. This is evidence in favor of communicating hydrocele of the testicular membranes. Enlargement of the scrotum is sometimes also observed with tension or “inflating” of the abdomen.
Subjective sensations are insignificant. Complaints are rare. In case of acute, infected or tense dropsy, pain may be observed.
To establish the correct diagnosis, ultrasound is used - ultrasound examination of the inguinal canals and scrotal organs and duplex examination of testicular vessels.
Ultrasound often makes it possible to detect a problem from the other side - for example, an inguinal hernia or spermatic cord cyst that is invisible during examination.
Sometimes enlargement of the scrotum and groin area appears and disappears, and may be absent upon examination by a doctor. Then a photograph taken when a swelling appears in the scrotum or groin area, taken by the parents, helps resolve the issue of diagnosis.
Diagnosis of varicocele
During the examination, the doctor palpates the scrotum. In order to determine the form of dropsy (communicating or non-communicating), the child is first examined in an upright position, and then in a lying position. In a case in which the size of the dropsy decreases in a supine position, we can talk about the presence of communication between the abdominal cavity and the scrotal cavity. This form of pathology is also supported by an enlargement of the scrotum when coughing.
Instrumental diagnostic methods include:
- Diaphanoscopy (examination of tissues in transmitted light). As a result of the examination, both liquid (it evenly transmits light) and part of the intestine or omentum (they block the light flux) can be detected in the scrotum. This indicates the presence of an inguinoscrotal hernia.
- Ultrasound examination of the scrotum and inguinal canals. The technique provides the opportunity for more accurate diagnosis, incl. exclude or confirm torsion of the testicle or its epididymis, testicular neoplasms, and also determine the type of hydrocele.
Diseases and circumstances that are often accompanied by the occurrence of hydrocele
- Cryptorchidism (undescended testicle)
- Hypospadias
- False hermaphroditism
- Epispadias and exstrophy
- Ventriculo-peritoneal shunt
- Prematurity
- Low birth weight
- Liver diseases with ascites
- Defects of the anterior abdominal wall
- Peritoneal dialysis
- Burdened heredity
- Cystic fibrosis
- Inflammatory diseases of the scrotum leading to the development of reactive hydrocele
- Testicular torsion
- Injury
- Infection
- Previous operations affecting the lymphatic system of the testicle
Treatment of hydrocele (hydrocele) and lymphocele without surgery. Duration of observation.
Hydrocele in children under 1 year of age requires observation by a pediatric urologist-andrologist. If fluid accumulates and tension appears in the membranes of the testicle, punctures are performed to remove hydrocele. Sometimes repeated punctures are required.
Communicating hydrops with a narrow peritoneal process is usually observed up to 2 years.
Observation is also required for traumatic dropsy, which occurs as a result of a bruise without compromising the integrity of the testicle. As a rule, 3 months are enough to assess the dynamics of the process and, if there is no improvement, prescribe surgical treatment. The same applies to hydrocele formed after inflammation.
The most difficult is the management of patients with lymphocele that forms after surgical treatment of an inguinal hernia and varicocele. In this case, prematurely performed surgery has little chance of success. For 6-12 months, it is necessary to monitor the condition of the testicle according to ultrasound and duplex examination of the scrotal organs in order to assess the dynamics of the process and the effectiveness of the therapy.
Hydrocele (hydroxycele) - symptoms and treatment
First of all, when treating hydrocele, it is necessary to make an accurate diagnosis in a timely manner. In children in the first two years of life in the presence of hydrocele, conservative therapy and expectant management are recommended [1][2][3][9]. Drug therapy is not required at this time. Hydrocele usually disappears during the first year of a child’s life, so surgical treatment in most cases is not indicated; only dynamic observation by a pediatric surgeon or urologist is required [1][2][3]. Taking into account modern clinical recommendations, early surgical treatment is indicated only if a concomitant inguinal hernia or testicular pathology is suspected.
However, if the hydrocele does not go away within two years of the baby's birth, surgery will be required. If the hydrocele is not surgically removed at an older age, it can continue to grow. Surgery is recommended for all children with hydrocele over the age of 2 years as a planned procedure.
Drug therapy may be required for isolated hydrocele in children against the background of acute epididymitis and orchitis, and for allergic edema of the scrotum. In such cases, rest, wearing a bandage to immobilize the scrotal organs, antimicrobial and desensitizing drug therapy are required [6].
The most radical and effective method of treating hydrocele is surgical treatment. First of all, these are open surgical interventions :
- Bergman operations;
- Winkelmann operation;
- plication (reduction in size) of the testicular membranes;
- Lord's operation;
- plasma coagulation of the tunica vaginalis of the testicle [4].
These are minimally invasive operations with video assistance for excision of testicular membranes. The main objective of most of the listed methods is aimed at eliminating the serous cavity between the plates of the tunica vaginalis of the testicle. The operation performed must meet certain requirements:
- do not relapse;
- be minimally invasive;
- do not cause complications;
- do not cause testicular dysfunction;
- the subsequent period of hospitalization should be short.
For hydrocele of the testicular membranes, in most clinics in Russia, preference is given to three types of open surgical interventions:
Winkelmann operation. During this surgical intervention, one of the layers of the testicular membrane is cut along the anterior surface, turned inside out and sutured behind the testicle. In this case, fluid accumulation no longer occurs. This operation consists of making a 4–5 cm long incision on the anterior
the surface of the scrotum on the side of the presence of hydrocele. All membranes are dissected up to the vaginal membrane. The testicle is removed into the wound. Next, puncture of the vaginal membrane and evacuation of fluid is carried out. Then this membrane is also cut and the testicle is exposed. The testicle and its epididymis are examined.
Next, plastic surgery of the testicular membranes is performed according to Winkelmann: the membranes are everted and stitched. The fluid produced by the epithelium of the tunica vaginalis of the testicle will be absorbed by the surrounding tissues. Next, the testicle is immersed in the wound, a layer-by-layer suture of the wound is made, leaving a drainage half-tube, which is removed the next day after the operation, and a tight bandage is applied. Sutures are removed on the 10th day after surgery.
Bergman's operation. A skin incision is made above the dropsy. The hydrocele is cleared of fascia and pierced with a trocar; the serous fluid is collected in a prepared container. The testicular membranes are excised, careful hemostasis is performed, and the testicle is again placed in its bed. A drainage is installed under the testicle. The skin is sutured with antibacterial, self-absorbing, cosmetic material that does not leave scars. An aseptic dressing is applied. A correctly performed Bergman operation eliminates the possibility of complications. Damage to the spermatic cord during Bergmann's operation is also excluded. In the postoperative period, antibacterial drugs are prescribed. It is necessary to wear a suspensor for some time.
Lord's Operation . During this operation, the testicular membranes are dissected, the hydrocele is released, and the vaginal membrane around the testicle is corrugated. In this case, the testicle itself is not freed from the surrounding tissues and does not dislocate into the wound. This allows you to reduce trauma to adjacent tissues and feeding vessels of the testicle.
In 2005, a method of plasma coagulation of the tunica vaginalis of the testicle [11]. This method is based on the effect of a plasma flow (ionized inert gas argon) on the vaginal membrane of the testicle. However, the method has not received widespread use [4].
Laparoscopic closure of the opening of the tunica vaginalis of the testicle is one of the surgical treatment options, however, the use of laparoscopy in the treatment of hydrocele in children remains controversial, as there is a risk of relapses and complications associated with the duration of anesthesia [12].
Sclerotherapy occupies a special place among surgical minimally invasive methods of treating hydrocele [4]. Serous fluid is sucked out with various instruments (primarily a syringe), for this purpose a puncture of the hydrocele is performed. After removing the fluid, sclerosing drugs are injected into the cavity. The basis of their mechanism of action is the stimulation of an inflammatory cellular response to the introduction of a chemical substance. In the future, this leads to sticking of the layers of the vaginal membrane. For sclerotherapy for hydrocele, various substances are used, such as:
- tetracycline;
- betadine (polyvidone-iodine);
- polidocanol;
- sodium tetradecyl sulfate;
- ethanolamine;
- phenol;
- 96% ethyl alcohol [4].
Sclerotherapy is somewhat less effective than open surgery. It can be used to a limited extent in elderly people, as well as with large hydroceles. Elimination of dropsy by puncture without the administration of sclerosing drugs is temporary. The hydrocele puncture method is currently not used due to the high risk of infection of the hydrocele [1][2][3][6].
Complications are possible after surgical treatment - any surgical intervention carries this risk. After surgical treatment of hydrocele, bleeding may occur, hematomas, swelling and suppuration may form [9][10].
When is surgery performed for hydrocele?
- Operations for communicating hydrocele of the testicle are most often performed in children aged 2 years.
- From 1 to 2 years, operations for communicating hydrops are performed if:
- combined dropsy and inguinal hernia
- when the volume of the scrotum clearly changes with changes in body position
- dropsy increases, causing discomfort
- infection joins
- Surgeries for post-traumatic dropsy – 3-6 months after injury.
- Lymphocele that occurs after surgery for an inguinal hernia or varicocele is operated on 6 to 18 months after the appearance of fluid in the membranes of the testicle.
Surgery for hydrocele (hydrocele). Surgical options.
The type of operation depends on the age of the patient and the characteristics of the dropsy.
Surgery for communicating hydrocele of the testicle. Operation Ross.
For communicating dropsy, as a rule, the Ross technique is used - isolation from the elements of the spermatic cord, excision and ligation of the internal inguinal ring of the peritoneal process, as well as the formation of a “window” in the membranes of the testicle. The operation is performed through a small incision in the groin area.
The operation is delicate, requiring good technique - careful and careful preparation while preserving all the anatomical formations of the spermatic cord - the vas deferens and testicular vessels, as well as the inguinal nerve.
Laparoscopic operations are sometimes used for testicular hydrocele, but the morbidity, risk of relapses and complications when using them are higher, and the duration of anesthesia is longer, so they are not widely used.
Operations for isolated hydrocele of the testicular membranes and lymphocele in children and adolescents.
Isolated hydrocele and lymphocele are indications for Bergman's operation - excision of the inner membranes of the testicle from the scrotal approach. In cases of large hydroceles and lymphoceles, drainage is often left in the wound and pressure bandages are applied.
Winkelmann's operation is a dissection of the testicular membranes in front and suturing the resulting edges of the membranes behind the epididymis. Currently used rarely due to changes in the appearance of the scrotum and testicular contours.
Among the complications, the most common is recurrence of dropsy (5-20%), which in case of lymphocele can reach 70%. A particularly high percentage of relapses is observed when operations are not performed on time.
Complications of operations.
The overall risk of complications ranges from 2 to 8%.
Relapses of dropsy occur with a frequency of 0.5 to 6%. In adolescence, relapses of dropsy are more common.
The risk of infertility after such operations is due to surgical trauma and averages about 2-5% and mainly depends on the technique of performing the intervention.
Infertility is not always a manifestation of damage to the vas deferens. In 5-8% of patients, there are rudiments of the rudiments of the female genital organs, which indicate the presence of more or less pronounced defects of the reproductive system that arise in utero or are genetically predetermined.
One of the complications is high fixation of the testicle, when the testicle is pulled up to the inguinal canal and is subsequently fixed there with scar adhesions.
Testicular atrophy can be observed due to impaired blood circulation in the testicle, which occurs during mobilization of the peritoneal process from the elements of the spermatic cord.
Unpleasant or painful sensations in the area of the wound or scrotum on the side of the operation - hyperesthesia associated with pinching in the scar or damage to nerve endings. These phenomena usually disappear 6-12 months after surgery.
Prevention of complications.
The development of complications can be prevented by a high level of surgical technology and timely determination of indications for surgical treatment.
Postoperative period
Surgeries for dropsy are usually well tolerated by children and do not significantly interfere with their movements. However, with sudden movements or constipation as a result of increased intra-abdominal pressure or direct impacts, the formation of hematomas in the scrotum and groin area is possible. Therefore, children should limit their activity until the postoperative wound heals and follow a diet.
On the first day after surgery, non-narcotic painkillers (analgin, paracetamol, ibuprofen, Panadol and others) are usually prescribed. Laxatives are used for 4-5 days after surgery.
For 2 weeks after surgery, do not wear underwear that compresses the scrotum to avoid pushing the testicle up toward the inguinal canal, due to possible fixation of the testicle above the scrotum.
School-age children are exempt from physical education for 1 month.
Price and cost of surgery for hydrocele in children
| Service | price, rub. |
| Surgical treatment of hydrocele of 1st category of complexity | 37000 |
| Surgical treatment of hydrocele of 2nd category of complexity | 49000 |
| Surgical treatment of hydrocele of 3rd category of complexity | 63000 |
The cost of the operation includes (no additional payment for services is necessary!):
- inpatient accommodation 1 day double room with all amenities
- preoperative tests
- disposable suture material Vicryl, PDS
- application of intradermal cosmetic suture
- disposable surgical consumables
- surgical instruments Ceatec GmbH Germany
- microsurgical instruments and equipment
- constant telephone communication with the attending physician
- examination any day in the clinic within 14 days after surgery
The cost of the operation does not include: anesthesia, additional diagnostics and treatment of concomitant diseases and their complications.
Anesthesiological support: anesthesiological apparatus Drager Fabius Plus (Germany), combined general anesthesia (inhalation anesthesia, caudal/local anesthesia).
** This is not a public offer agreement. Check the cost of services on the day of your request.
Don't waste your precious time - call!
Our specialists will be happy to answer all your questions
+7
Our advantages
Experienced surgeons
Individual approach
Without pain and fear
Comfortable conditions