Anastasia Safina (author of the publication)
The question “how to behave correctly during childbirth?” worries most expectant mothers, because everyone wants to do everything right. I, Anastasia Safina, will tell you what mistakes during childbirth can harm the mother and baby.
Although childbirth is a natural physiological process, the expectant mother should be aware of and, if possible, control her behavior during contractions and pushing. This will help her survive childbirth easier, and the baby will be born healthy. From the article you will learn what not to do during childbirth, so as not to complicate the task for yourself and obstetricians.
Don't squeeze during contractions
Contractions are involuntary contractions of the uterine muscles that allow the cervix to open. Although the process is quite painful, you should not be scared or strain your body. Tension will cause the pain to become more intense. Squeezing the pelvic floor muscles can provoke spasm of the cervix - then even painful and intense contractions will not contribute to the opening of the birth canal.
If you feel that the strength and dynamics of contractions are increasing, do not be alarmed. Remember that childbirth is a natural process and the pain during it will not be so unbearable that you will not be able to survive it. Try to relax your body as much as possible, trust it. Think about the fact that your body is now working to open the birth canal and try not to interfere with it. It is helpful to learn various breathing techniques in advance to help you relax and relieve pain. The less tension in the body, the lower the degree of pain. You can learn more about breathing during childbirth in the courses of our online school “Easy Childbirth”.
Breathing during childbirth: pushing
The breathing and behavior of a woman in labor during pushing is usually controlled by a midwife: she tells you when and how to push, and when you need to “breathe” through the pushing. If we talk about general principles, breathing during pushing looks like this: take a deep breath through your nose and exhale through your mouth, sharply, aimed at the uterus and pushing out the baby, and not at the head.
If you are going into labor, the correct breathing video you watched during pregnancy should appear before your eyes. When the contraction begins, relax as much as possible, take a deep breath and exhale slowly, and if necessary, do dog breathing. Practice proper breathing in advance - this will make the birth process much easier.
Read us on Yandex Zen
You can't shout
When the muscles of the uterus contract, the uterine vessels that feed the placenta are compressed. As a result, their lumen narrows, and the baby receives less oxygen. While screaming, you exhale and hold your breath for a while. By doing this, you deprive the body of oxygen, which only increases hypoxia in the child.
Screaming during contractions deprives the woman in labor and increases the risk of ruptures, as the muscles of the pelvic floor and perineum become tense. In addition, shouting may prevent you from hearing important instructions from your doctor.
Lying on your back for a long time during contractions
In the supine position, the uterus and fetus compress the aorta and inferior vena cava. This seriously impedes blood flow to the heart, brain, uterus and fetus. As a result, the child experiences oxygen starvation, and blood stagnation occurs in the internal organs of the pregnant woman. A woman’s blood pressure drops, she experiences weakness, dizziness, and loses strength.
In between contractions, you can walk, sit, and constantly change your position. This improves the passage of the fetus and helps it take the correct position.
How to breathe properly and relax during childbirth
to give birth easily without complications?
Register for our free master class
and immediately after registration you will receive a free video lesson “How to relieve pain in childbirth?”
Get it for free
Abdominal prolapse
It begins several weeks before labor begins. When the baby prepares to be released, he presses his head against the lower part of the uterus and pulls it down. If previously the uterus was in the abdominal region, now it is in the pelvis. The fundus of the uterus begins to put pressure on the organs in the peritoneum and chest.
When moving, the discomfort usually stops being so intense.
Prolapse of the abdomen and uterus is usually accompanied by some symptoms.
Most often women experience:
- heartburn and belching (because the uterus puts pressure on the stomach and diaphragm);
- there is a frequent false urge to urinate (the uterus presses on the bladder).
Severe abdominal prolapse is usually observed only during the first birth. In all cases, the uterus drops just before the birth itself, or this symptom does not exist at all. You may also experience discomfort in the sacral area. They usually appear after the mucus plug comes out. Discomfort and pulling sensations disappear after rupture of the amniotic sac, because the pressure on the internal organs is eliminated.
Push prematurely
You should not give in to the first urge to push if the doctor has not told you that it is time. You can push when the birth canal is completely open and the baby's head is in the correct position. If the cervix is not fully dilated, pushing will cause serious tissue tears. When the baby's head is at the beginning of the birth canal, pushing can injure him.
To avoid such consequences, I recommend learning in advance breathing techniques that allow you to stop the pushing. Frequent shallow breathing causes the diaphragm to constantly move up and down, making pushing impossible.
Don't sit on a hard surface
Sitting on a hard surface significantly complicates the passage of the fetus through the birth canal. This is especially true for the period when contractions have already become quite strong and frequent. At this stage, the baby’s head enters the birth canal, and in a sitting position the process is complicated by excessive pressure from muscles and tissues. This constrains the baby’s movements, preventing him from taking the desired position.
You can help the baby move into the birth canal by moving your hips from side to side. They can be done comfortably while standing or sitting on a fitball.
Out-of-hospital birth: emergency measures at the prehospital stage
Childbirth is the physiological process of expulsion of the fetus, membranes and placenta through the mother's birth canal.
A doctor, paramedic or midwife of emergency and emergency medical care (E&E) may be faced with any period of labor: dilation, expulsion, the afterbirth and early postpartum period.
A health worker must be able to diagnose periods of labor, assess their physiological or pathological course, find out the condition of the fetus, choose rational tactics for managing labor and the early postpartum period, prevent bleeding in the placenta and early postpartum period, and be able to provide obstetric care for cephalic presentation.
Childbirth outside a hospital most often occurs during premature pregnancy or during full-term pregnancy in multiparous women. In such cases, they usually proceed rapidly.
There are premature, urgent and delayed births.
A birth that occurs between 22 and 37 weeks' gestation and results in premature babies is considered premature. Premature babies are characterized by immaturity, their body weight ranges from 500 to 2500 g, length from 19–20 to 46 cm.
Childbirth that occurs during a gestational age of 40 ± 2 weeks and ends with the birth of a live, full-term fetus weighing approximately 3200–3500 g and a length of 46 cm is considered urgent.
Childbirth that occurs during a gestation period of more than 42 weeks and ends in the birth of a fetus with signs of postmaturity (dense skull bones, narrow sutures and fontanelles, pronounced desquamation of the epithelium, dry skin) is considered post-term. Childbirth with a post-term fetus is characterized by a high percentage of birth injuries.
There are physiological and pathological childbirths. A complicated course of labor develops in pregnant women with extragenital pathology, a burdened obstetric-gynecological history, or a pathological course of pregnancy.
Therapeutic and tactical measures for workers of the S&NMP
- Resolve the issue of the possibility of transporting a woman in labor to the maternity hospital.
- Assess general and obstetric history data: the number of pregnancies and births in history, their course, the presence of complications.
- Determine the course of this pregnancy: threat of miscarriage, general weight gain, blood pressure dynamics, changes in blood tests (according to the exchange card).
- Analyze data from a general objective study.
- Assess the period of labor: the onset of contractions, their regularity, duration, intensity, pain. Carry out 4 external examinations and determine the height of the uterine fundus, the position and position of the fetus, the nature of the presenting part and its relationship to the plane of the entrance to the pelvis (movable above the entrance to the pelvis, fixed by the small segment, the large segment at the entrance to the pelvis, in the cavity of the small pelvis, on the pelvic floor). Auscultate the fetus.
- Assess the nature of the discharge: the presence of bloody discharge, leakage of amniotic fluid, the presence of meconium in it.
- If necessary, perform a vaginal examination.
- Diagnose childbirth:
- first or repeated;
- urgent, premature or late;
- period of childbirth - dilation, expulsion, afterbirth;
- the nature of the rupture of amniotic fluid - premature, early, timely;
- complications of pregnancy and childbirth;
- features of obstetric and gynecological history;
- concomitant extragenital pathology.
- If conditions and transportation possibilities are available, hospitalization in an obstetric hospital.
If it is not possible to transport the woman in labor to the maternity hospital, labor management should begin. The woman is given a cleansing enema, the pubic hair is shaved, the external genitalia are washed with boiled water and soap, the bed linen is changed, under which an oilcloth is placed, and a homemade pad is prepared - a small pillow wrapped in several layers of sheets (preferably sterile). During childbirth, the pad is placed under the pelvis of the woman in labor: thanks to the elevated position, free access to the perineum opens.
From the moment of complete or almost complete dilatation of the cervix, the forward movement of the fetus begins along the birth canal (biomechanism of childbirth). The biomechanism of childbirth is a set of translational and rotational movements that the fetus produces as it passes through the birth canal.
The first point is that as labor progresses, the head is inserted in one of the oblique sizes of the entrance to the small pelvis: in the first position - in the right oblique size, in the second - in the left oblique size. The sagittal suture is located in one of the oblique sizes, the leading point is the small fontanel. The head is in a state of moderate flexion.
The second point is the internal rotation of the head (rotation). In a state of moderate flexion in one of the oblique dimensions, the head passes through the wide part of the pelvic cavity, beginning an internal rotation that ends in the narrow part of the small pelvis. As a result, the fetal head changes from an oblique size to a straight one.
The rotation of the head is completed when it reaches the exit cavity from the pelvis. The fetal head is installed with a straight arrow-shaped suture: the third moment of the biomechanism of childbirth begins.
The third point is extension of the head. Between the pubic symphysis and the suboccipital fossa of the fetal head, a fixation point is formed, around which the head is extended. As a result of extension, the crown, forehead, face and chin are sequentially born. The head is born with a small oblique size of 9.5 cm and a corresponding circumference of 32 cm.
The fourth point is the internal rotation of the shoulders and the external rotation of the head. After the birth of the head, internal rotation of the shoulders and external rotation of the head occur. The fetal shoulders produce an internal rotation, as a result of which they are installed in the direct size of the pelvic outlet in such a way that one shoulder (anterior) is located under the pubis, and the other (posterior) is facing the coccyx.
The born fetal head turns with the back of the head towards the mother's left thigh (in the first position) or towards the right thigh (in the second position).
A fixation point is formed between the anterior shoulder (at the point of attachment of the deltoid muscle to the humerus) and the lower edge of the pubis. The fetal body flexes in the thoracic region and the posterior shoulder and arm are born, after which the rest of the body is easily born.
The forward movement of the fetal head at the end of the second stage of labor becomes noticeable to the eye: a protrusion of the perineum is detected, increasing with each attempt, as a result of which the perineum becomes more extensive and somewhat cyanotic. The anus also begins to bulge and gape, the genital slit opens and at the height of one of the attempts, the lowest segment of the head is shown from it, in the center of which is the leading point. With the end of the attempt, the head disappears behind the genital slit, and with a new attempt it reappears: cutting in of the head begins, indicating that the internal rotation of the head ends and its extension begins.
Soon after the end of the pushing, the head does not go back behind the genital slit: it is visible both during the pushing and outside the latter. This condition is called eruption of the head. The eruption of the head coincides with the third moment of the biomechanism of childbirth - extension. By the end of extension of the head, a significant part of it has already emerged from under the pubic arch. The occipital fossa is located under the pubic symphysis, and the parietal tubercles are tightly covered by highly stretched tissues that form the genital fissure.
The most painful, albeit short-lived, moment of childbirth begins: when pushing, the forehead and face pass through the genital slit, from which the perineum slides off. This ends the birth of the head. The latter makes its outer turn, the head being followed by the shoulders and torso. The newborn takes its first breath, screams, moves its limbs and begins to quickly turn pink.
During this period of labor, the condition of the woman in labor, the nature of labor, and the fetal heartbeat are monitored. The heartbeat must be heard after each effort; You should pay attention to the rhythm and sonority of the fetal heart sounds. It is necessary to monitor the progress of the presenting part - during the physiological course of labor, the head should not stand in the same plane of the small pelvis for more than 2 hours, as well as the nature of the discharge from the genital tract (during the period of opening and expulsion of bloody discharge from the genital tract there should be no).
As soon as the head begins to cut in, that is, at the moment when, when an attempt appears, it appears in the genital slit, and with the end of the effort it goes into the vagina, you must be ready to give birth. The woman in labor is placed across the bed, her head is placed on a bedside chair, and a homemade pad is placed under the pelvis. Another pillow is placed under the mother's head and shoulders: it is easier to push in a semi-sitting position.
The external genitalia are washed again with warm water and soap and treated with a 5% iodine solution. The anus is covered with sterile cotton wool or a diaper.
The person delivering the baby thoroughly washes his hands with soap and treats them with a disinfectant solution; It is advisable to use a sterile disposable obstetric kit.
Accompanying childbirth involves providing obstetric care.
In case of cephalic presentation, obstetric aid during childbirth is a set of sequential manipulations aimed both at promoting the physiological mechanism of labor and at preventing injuries to the mother and fetus.
As soon as the head crashes into the genital slit and maintains this position even outside the contraction, the eruption of the head begins. From this moment, the doctor or midwife, standing to the right of the woman in labor, sideways to her head, with the palm of her right hand with her thumb held wide apart, clasps the perineum, covered with a sterile napkin, through which she tries to delay the premature extension of the head during contractions, thereby facilitating the emergence of the back of the head from under the symphysis . The left hand remains “ready” in case the forward movement of the head turns out to be too strong and the right hand alone would not be able to hold it. As soon as the suboccipital fossa fits under the pubic arch (the person delivering the baby feels the back of the head in the palm of his hand), and the parietal tubercles are palpated from the sides, they begin to remove the head. The woman in labor is asked not to push; with the palm of the left hand they clasp the protruding part of the head, and with the palm of the right hand with the thumb abducted they clasp the perineum and slowly, as if removing it from the head (from the face), at the same time with the other hand they carefully lift the head up - at the same time, first the forehead, then the nose are shown above the perineum , mouth and finally chin. It is absolutely necessary to withdraw the head until the perineum “comes off” from the chin, that is, until the chin comes out. All this must be done outside of a contraction, since during a contraction it is very difficult to slowly remove the head, and with rapid withdrawal the perineum is torn. At this moment, the flowing mucus should be sucked out of the fetal mouth, since the child may take the first breath, as a result of which the mucus can enter the respiratory tract and cause asphyxia.
After the head is born, a finger is drawn along the fetal neck to the shoulder: check whether the umbilical cord is wrapped around the neck. If there is an entanglement of the umbilical cord, the loop of the latter is carefully removed through the head.
The born head usually turns with the back of the head towards the mother's thigh; sometimes external rotation of the head is delayed. If there are no indications for the immediate end of labor (intrauterine asphyxia of the fetus, bleeding), one should not rush: one must wait for the independent external rotation of the head - in such cases, the woman is asked to push, while the head is turned with the back of the head towards the mother’s thigh and the front shoulder comes under the womb.
If the front shoulder does not fit under the womb, help is provided: the turned head is grabbed between both palms - on one side by the chin, and on the other - by the back of the head, or they place their palms on the temporo-cervical surfaces and carefully, easily rotate the head with the back of the head towards the position, at the same time carefully pulling it down, bringing the front shoulder under the pubic symphysis.
Next, they clasp the head with their left hand so that its palm rests on the lower cheek and lift the head, and with their right hand, just as they did when removing the head, they carefully move the perineum from the back shoulder.
When both shoulders are out, they carefully grab the baby by the body in the armpit area and, lifting it up, remove it completely from the birth canal.
The principle of “protecting the perineum” in anterior occipital presentation is to prevent premature extension of the head; only after the back of the head comes out and the suboccipital fossa rests on the lunar arch, the head is slowly released above the perineum - this is an important condition for preserving the integrity of the perineum and the birth of the head in the smallest size - small oblique. If the head erupts in the genital slit not at a small oblique size (with an occipital presentation), it can easily rupture.
Birth trauma of the newborn (intracranial hemorrhage, fractures) can often be associated with the technique and method of childbirth.
If obstetric manual assistance during the eruption of the head is carried out roughly (or the person delivering the baby presses on the head with his fingers), this can lead to these complications. To avoid such complications, it is recommended to eliminate the excessive back pressure of the stretching perineum on the fetal head, for which the operation of dissecting the perineum is used - perineo- or episiotomy.
Obstetric manual assistance during eruption of the head should always be as gentle as possible. It aims, first of all, to help the birth of a healthy child, without causing any trauma to him, and at the same time to preserve the integrity of the pelvic floor as much as possible. This is the only way to understand the term “perineal protection.”
Immediately after the birth of the head, mucus and amniotic fluid must be sucked out from the upper parts of the pharynx and nostrils using a pre-boiled rubber bulb. To avoid aspiration of stomach contents, the newborn's throat is first cleared, and then the nose.
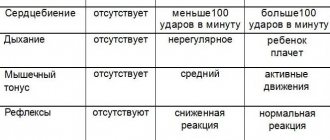
The newborn baby is placed between the mother's legs on sterile diapers, covered with another one on top to prevent hypothermia. The child is examined and assessed using the Apgar method immediately at birth and after 5 minutes (Table). The Apgar method of assessing the condition of the fetus allows you to make a quick preliminary assessment of five signs of the physical condition of the newborn: heart rate - using auscultation; breathing - when observing the movements of the chest; baby's skin color - pale, cyanotic or pink; muscle tone - by the movement of the limbs and reflex activity when spanking the plantar side of the foot.
A score of 7 to 10 (10 points indicates the best possible condition of the infant) does not require resuscitation.
A score from 4 to 6 indicates that these children are cyanotic, have arrhythmic breathing, weakened muscle tone, increased reflex excitability, a heart rate above 100 beats/min and can be saved.
A score from 0 to 3 indicates the presence of severe asphyxia. Such children at birth should be classified as requiring immediate resuscitation.
0 points corresponds to the concept of “stillborn”.
Assessment at 1 minute after birth (or earlier) should identify infants who require immediate care, and assessment at 5 minutes correlates with neonatal morbidity and mortality.
After the first cry and respiratory movements appear, 8–10 cm away from the umbilical ring, the umbilical cord is treated with alcohol and cut between two sterile clamps and bandaged with thick surgical silk and a thin sterile gauze ribbon. The umbilical cord stump is lubricated with a 5% iodine solution, and then a sterile bandage is applied to it. You cannot use a thin thread to tie the umbilical cord - it can cut through the umbilical cord along with its vessels. Immediately, bracelets are placed on both arms of the child, which indicate his gender, surname and first name of the mother, date of birth and birth history number.
Further treatment of the newborn (skin, umbilical cord, prevention of ophthalmoblenorrhea) is carried out only in an obstetric hospital, under conditions of maximum sterility to prevent possible infectious and purulent-septic complications. In addition, inept actions during secondary processing of the umbilical cord can cause difficult-to-control bleeding after cutting the umbilical cord from the umbilical ring.
The woman in labor is drained of urine using a catheter and begins to manage the third stage of labor.
Management of the afterbirth period
The afterbirth period is the time from the birth of the child until the birth of the placenta. During this period, the placenta, along with its membranes, is detached from the uterine wall and the placenta with membranes is born - the placenta.
During the physiological course of labor in the first two periods (dilation and expulsion), placental abruption does not occur. The succession period normally lasts from 5 to 20 minutes and is accompanied by bleeding from the uterus. A few minutes after the birth of the child, contractions and, as a rule, bloody discharge from the genital tract occur, indicating detachment of the placenta from the walls of the uterus. The fundus of the uterus is located above the navel, and the uterus itself, due to gravity, deviates to the right or left; At the same time, there is an elongation of the visible part of the umbilical cord, which is noticeable by the movement of the clamp placed on the umbilical cord near the external genitalia. After the birth of the placenta, the uterus goes into a state of sharp contraction. Its bottom is located in the middle between the pubis and the navel and is palpated as a dense, round formation. The amount of blood lost in the afterbirth period should usually not exceed 100–200 ml.
After the birth of the placenta, the woman who has given birth enters the postpartum period. Now she is called a postpartum woman.
Management of the subsequent period of labor is conservative. At this time, you cannot be away from the woman in labor for even a minute. It is necessary to monitor whether everything is fine, that is, whether there is any bleeding - both external and internal; it is necessary to monitor the nature of the pulse, the general condition of the woman in labor, and signs of placental separation; urine should be removed, since a full bladder interferes with the normal course of the afterbirth period. To avoid complications, it is not allowed to perform external massage of the uterus or pull the umbilical cord, which can lead to disruption of the physiological process of placenta separation and severe bleeding.
The baby's place coming out of the vagina (placenta with membranes and umbilical cord) is carefully examined: it is laid out flat with the maternal surface facing up. Attention is paid to whether all placental lobules have come out, whether there are additional placental lobules, whether the membranes have completely separated. Retention of parts of the placenta or its lobules in the uterus does not allow the uterus to contract well and can cause hypotonic bleeding.
If the placental lobule or part thereof is missing and there is bleeding from the uterine cavity, you should immediately perform a manual examination of the walls of the uterine cavity and remove the retained lobule by hand. If there is no bleeding, the missing membranes do not need to be removed: usually they come out on their own in the first 3-4 days of the postpartum period.
The born placenta must be taken to an obstetric hospital for a thorough assessment of its integrity by an obstetrician.
After childbirth, the external genitalia are toileted and disinfected. The external genitalia, vaginal opening and perineum are examined. Existing abrasions and cracks are treated with iodine; ruptures must be repaired in a hospital setting.
If there is bleeding from soft tissues, it is necessary to apply sutures before transport to an obstetric hospital or apply a pressure bandage (bleeding from a rupture of the perineum, clitoral area), vaginal tamponade with sterile gauze pads is possible. All efforts during these manipulations should be aimed at urgent delivery of the postpartum woman to the obstetric hospital.
After giving birth, the postpartum woman should be changed into clean linen, placed on a clean bed, and covered with a blanket. It is necessary to monitor the pulse, blood pressure, condition of the uterus and the nature of the discharge (bleeding is possible); you should give the woman hot tea or coffee. The placenta, the mother and the newborn must be taken to the obstetric hospital.
A. Z. Khashukoeva, Doctor of Medical Sciences, Professor Z. Z. Khashukoeva, Candidate of Medical Sciences M. I. Ibragimova, Candidate of Medical Sciences M. V. Burdenko, Candidate of Medical Sciences Russian State Medical University, Moscow
Ignore the obstetrician's instructions
Even if you have thoroughly prepared for childbirth, studied many topical articles, and mastered breathing techniques, do not neglect the doctor’s recommendations. No matter how hard you try, you will still not be able to take into account all the relevant factors, simply because you do not have a medical education. In addition, the psycho-emotional state of a woman during childbirth prevents her from correctly assessing the situation and making the right decision.
Try to trust the medical staff, it will be easier for both you and them. To make this easier, it is better to choose a doctor and maternity hospital in advance.
Relaxation and Relaxation Techniques
The ability to relax helps to cope with muscle tension, pain in the lower back and legs, and allows you to have a positive outlook on childbirth. Stress negatively affects both the condition of the woman herself and the health of the unborn child. The right relaxation technique will help you get rid of stress.
You can relax with the help of yoga, meditation, and specially developed techniques for pregnant women. For example, Jacobson's progressive muscle relaxation method. It is based on the change of tense and relaxed states and allows you to relax all muscle groups in turn. Relaxation exercises should be done once or twice a day.
You can’t strain your face or puff out your cheeks
To make the birth go smoothly and make it easier for the fetus to move through the birth canal, you need to push correctly. This means that when you take air into your lungs, you need to “swallow” it and tense the muscles of the anterior abdominal wall as much as possible. Instead, women sometimes tense their facial muscles and puff out their cheeks. Such an attempt is not effective; it does not help the baby move forward. In addition, due to excessive tension on the face, capillaries can burst.
Request pain relief if the doctor says it's too late
One of the most popular types of pain relief during childbirth is epidural anesthesia. It is placed on a woman in labor when the uterus is dilated by 5-6 cm. If it is placed later, then at the right moment the woman may not feel the urge to push and will not be able to push normally during childbirth. If possible, it is better to discuss with your doctor in advance whether you want to use anesthesia. And you can read more about it in our article.
How to behave in the delivery room?
The first contractions, ambulance, maternity hospital, doctors: everything happens so quickly that most women in labor simply panic from the surrounding bustle. To make labor as comfortable and easy as possible, follow these recommendations:
- Collect all the necessary things in advance: a change of clothes for yourself and your baby, food, personal hygiene products.
- Listen to the medical staff: try not to interrupt or shout, no matter how hard and scary it is for you. The doctor's main job is to help you. And also do not hesitate to ask questions.
- Breathe correctly - you need to master the breathing technique in advance, by the end of the third trimester, bringing the acquired skills to automaticity. This will help you calm down, reduce pain, and relieve the pain of contractions.
- Take a comfortable position - consult your doctor and take the most comfortable position to relieve pain during contractions.
- Try not to scream - this is very exhausting and takes away the strength that you will need during pushing.
- Don't be alone. If all the medical staff has left the office, and you feel unwell, do not hesitate to press the button and call a doctor. Childbirth is a case when it is better to play it safe.
- Do self-massage and massage - this will help relieve pain and reduce tension levels. If the birth is partnered, the massage should be done by the spouse.
- Push only at the doctor’s command - no matter how strong the desire, amateur efforts are unacceptable, as they can harm the baby.
Don't panic and despair
Childbirth is a truly exciting and difficult process. How everything goes depends 90% on the attitude of the expectant mother and her ability to maintain composure. If you feel contractions starting, don't panic. You still have enough time to call an ambulance and get to the maternity hospital. During the birth process, it is also important to maintain inner peace. If you are already tired of pushing and pain, then there is not much left. A little more and you will see your baby and be able to put him to your breast. Remember this in the most difficult moments.
Now you know what prohibitions exist during childbirth and why it is important to avoid mistakes. Maintain a positive attitude and composure, trust the medical staff, and your birth will go smoothly.
Did you like the post? Share it on social networks!
Telegram
Tweet
We recommend that you read similar articles:
- Main indications for cesarean section: when should it be done?
- Popular myths about pregnancy
- All about false contractions: causes, symptoms, how to distinguish