If the baby was born prematurely and his body weight is less than 2.5 kg, he needs special nutrition. The ideal option for him would be breast milk. Surprisingly, if a woman does not reach the time prescribed by nature, her milk changes slightly in composition, increasing its nutritional value several times over.
When, for objective reasons, breastfeeding is considered impossible, the question arises of feeding a premature baby with formula. It is not difficult to recognize such products in the line of many manufacturers - in most cases, the abbreviation PRE indicates a special composition.
Nutritional features for premature babies
For a baby who hastened to get acquainted with the world around him, special nutrition is required. Feeding premature infants with a formula of the required composition will allow them to quickly and painlessly approach standard body weight indicators. Baby food for such babies differs from conventional adapted formulas in several ways:
- • The composition should contain highly digestible milk protein and casein - whey protein.
• Maltodextrin and lactose act as carbohydrate components.
• The composition of the mixture must be enriched with vitamins and microelements necessary for full development - calcium, manganese, iodine, selenium, phosphorus.
• Formulas for low birth weight infants are characterized by an increased amount of polyunsaturated fatty acids.
• High nutritional value and calorie content are prerequisites for rapid weight gain.
• It is unacceptable to contain soy protein in the mixture, which significantly complicates the digestion process.
A high percentage of nutrients significantly reduces the possible shelf life. Feeding a premature baby with a formula of a special composition will not only quickly gain the missing weight, but will also ensure its proper development.
Which is better?
Finding the right mixture can be difficult. We have compiled for you a visual rating of the best formulas for premature babies.
Rating 2019
| Name and price | Age/Weight | Features of the composition | Advantages and disadvantages |
| Similac Neosure Similak NeoShur From 940 rub. | Up to 6 months; up to 2.5 kg. | Present:
| Of the minuses: increased gas formation and constipation are possible. Pros:
|
| NAN(PreNAN) NAS (PreNAN) From 940 rub. | Up to 7 months and beyond; up to 3.5 kg. | Present:
| Of the minuses:
Pros:
|
| Nutrilon (PreNutrilon 0) Nutrilon From 690 rub. | Up to 7 months; up to 3 kg. | Present: prebiotics, triglycerides, fish oil; vitamins and microelements, nucleotides, taurine, soy lecithin. | Of the minuses: high content of Zn and copper, which can increase the load on the baby’s heart, liver and kidneys. Pros:
|
| Hipp Pre (Hipp Pre) From 600 rub. | Up to 7 months; up to 3 kg. | Present:
| Of the minuses:
Pros:
|
| Nanny (with prebiotics) From 2100 rub. | Up to 12 months; up to 3.5 kg. | Present:
| Of the minuses:
Pros:
|
| Bellakt (Bellakt PR 0-12) From 600 rub. | Up to 12 months; up to 4 kg. | Present:
| Of the minuses:
Pros:
|
| FrisoPre (FrisoPre) From 500 rub. | Up to 12 months; up to 4 kg. | Present:
| Of the minuses:
Pros: Provides quick weight gain |
| Materna From 3000 rub. | Up to 12 months; up to 4 kg. | Present:
| Of the minuses: Allergic reactions to lactose are possible. Pros:
|
Other dry formulas - “Malyutka”, “Nestozhen”, “Similak Premium” and others - were not included in the rating, since the manufacturer’s line does not have a dedicated nutrition marked “for premature babies”.
You might be interested to know
What are the best bottles for premature babies?
How do you experience spontaneous childbirth with twins? Read in this article.
Nutrition system for a premature baby with low weight
Concerned about the low weight of their baby, parents are always interested in how much formula a premature baby should eat. Pediatricians are trying to warn them against trying to feed the little one. The intervals between daytime feedings should be approximately 2.5-3 hours, at night a little longer - 3-4 hours. Many mothers are sure that the more their child eats, the faster he will gain weight. However, you should trust the baby’s natural appetite, inherent in nature itself. It has been noticed that if a child eats forcefully, his growth even slows down.
It is important not only to be interested in what formula to feed premature babies, but also to organize the correct nutrition system. You need to rely not on the quantity of each serving, but on its calorie content. Every day it is necessary to increase the energy value of the product until the child’s weight approaches the required value. In order not to subsequently “overfeed” the baby, the calorie content of the product begins to be gradually reduced.
Differences from standard mixtures
When the child reaches a weight of 3000 g, he can eat regular formulas, but this transition must take place gradually, according to the scheme determined by the pediatrician. Before your baby reaches a healthy weight, you will need to feed him special foods.
Manufacturers mark their special mixtures with the prefix “Pre” or the mark “0”.
The main differences between this mixture and the usual one are:
- High calorie content. This allows you to gain the desired weight as quickly as possible. The child eats less, but gets full faster;
- A large amount of protein for weight gain. In addition, it develops muscles and strengthens bones;
- Casein included. Helps a child’s weak stomach digest food better, protects against constipation and colic;
- Prebiotics and nucleotides support healthy intestinal microflora;
- Polyunsaturated fatty acids guarantee normal development of the central nervous system;
- A complex of vitamins strengthens vision.
Some manufacturers add iron, zinc, manganese and other minerals to their formulations, which accelerate the growth and development of the baby.
Typically, premature infant formula contains lactose and palm oil. These substances accelerate the baby's growth, but can cause allergic reactions, so some manufacturers offer safer and healthier analogues.
For example, for children with lactose allergies, there are goat milk or soy milk formulas.
Range of infant formulas for premature babies
Getting acquainted with the range of modern baby food manufacturers, many mothers try to find out which formula is best for a premature baby. It would be much smarter not to rely on the opinions of other parents, but to try to independently analyze the products of well-known companies.
PRE Nutrilon
The mixture has the correct ratio of vitamin and mineral composition. The composition contains nucleotides that help strengthen the baby's immune system. Pediatricians note the least load on the metabolic system of an infant. As a rule, it does not cause an allergic reaction and even, according to parents, reduces the number of regurgitations.
PRE NAN
The peculiarity of the mixture is its high whey protein content. Contains fatty enzymes necessary for the baby's body. The formula is very well absorbed, and many parents, when asked which formula is best for premature babies, confidently point to this product.
Friso PRE
A characteristic feature of Frisopre is the presence of amino acids, nucleotides and a high percentage of iodine. According to parents' reviews, the product does not cause allergic reactions, intestinal colic or constipation. Among the shortcomings is the lack of light fats.
Nutrilak PRE
Excellently balanced composition of proteins, fats and carbohydrates, high content of vitamin E and folic acid to prevent anemia. In terms of its composition, “Nutrilak Pre” is an excellent example of what formulas for premature babies help to gain weight with the full development of the entire child’s body.
Similac Neo Sure
Does not contain palm oil, the composition contains all the necessary vitamins, microelements, fatty acids and nucleotides. Promote rapid weight gain without loss in the development of all body systems.
Feeding premature babies
Premature children represent a special group of patients who are characterized by signs of physiological immaturity, which determines special conditions for nursing. In the Russian Federation, the proportion of premature babies among all newborns averages 6–8%. Children born prematurely should constantly be the focus of attention of pediatricians, since it is among them that the highest percentage of perinatal pathology is observed and deviations in subsequent development are much more often detected [1].
The greater the degree of prematurity, the more significant problems associated with the subsequent development of the child have to be faced: they can vary from minimal brain dysfunction (behavior and learning problems, hyperactivity syndrome with impaired attention) to severe disorders leading to disability. Some violations are irreversible. The compensatory capabilities of the child’s body are quite large, but they are fully manifested only against the background of active rehabilitation, good care, and nutritious nutrition [2]. The rehabilitation carried out may be successful and lead to minimizing the consequences of prematurity, otherwise various deviations in the development of the child may arise. In this regard, the role of adequate nutrition of a premature baby - both in the earliest stages of its development and throughout the first year of life - can hardly be overestimated. In recent years, certain progress has been made both in improving methods of feeding very premature infants (parenteral and tube nutrition), and in improving the formulation of special adapted formulas for premature infants, in particular as a result of the introduction into their composition of nucleotides, long-chain polyunsaturated fatty acids, a number of those involved in metabolism of nervous tissue of amino acids, which have a positive effect on the development of the brain and visual organs [3].
The highest growth rates are observed in the fetus during uncomplicated pregnancy. But in premature and low birth weight babies, the period of intrauterine development is shortened, as a result of which a noticeable part of this important stage, which occurs extrauterinely, “falls out”. This affects the subsequent development of the child.
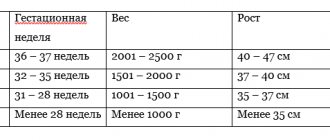
Babies born at less than 37 weeks (259 days) of gestation are considered premature. As a result of premature birth, the child is born insufficiently mature and has problems associated with adaptation to the conditions of extrauterine life. The situation is complicated by problems such as the immaturity of the digestive system and limited nutrient reserves in the body.
The supply of nutrients to the body before and after birth. During intrauterine development, the fetus constantly receives nutrients through the umbilical cord. Glucose, amino acids and fatty acids provide elemental nutrition. After birth, nutrition (breast milk) begins to be supplied orally, in the form of more complex compounds (lactose - proteins - lipids) that require enzymatic breakdown.
Premature infants, who are characterized by so-called “catch up growth” after stabilization of their clinical condition, have high nutrient requirements [4]. Meanwhile, the ability to assimilate them does not always correspond to the total needs of a premature baby for nutrients and energy.
The prescription of nutrition and the choice of feeding regimen in premature infants are dictated by taking into account the characteristics of the digestive system and the metabolism of basic nutrients [5]. In such infants, the sucking and swallowing reflex is reduced or completely absent, the secretion of gastric juice is reduced, there is insufficient production of pancreatic proteases, lipase and intestinal disaccharidases (especially lactase), but at the same time the activity of intestinal peptidases is quite high. The ability of bile to emulsify fatty acids is reduced. Contamination with hospital microflora in combination with slow and irregular intestinal motility causes a high incidence of dysbiotic disorders. Due to hypogalactia, a significant proportion of women who give birth prematurely often do not have the opportunity to provide their child with breast milk [6].
Features of the composition of breast milk after premature birth. Back in the 1980s. A number of studies have shown that breast milk from women who gave birth prematurely has a higher energy value and contains more protein (1.2–1.6 g per 100 ml), and a higher concentration of essential amino acids in its amino acid composition. The fat content in such milk is also higher, and it also has a higher level of essential fatty acids. At the same total level of carbohydrates, milk contains less lactose and more oligosaccharides. The composition of breast milk in women after premature birth is also characterized by a higher content of a number of protective factors, in particular lysozyme. Human milk is easily digestible and well tolerated by premature babies, which makes it possible to achieve the full volume of enteral nutrition at an earlier date compared to artificial feeding.
The undoubted advantages of breast milk include immune defense factors; it contains bifidogenic components (oligosaccharides), which have a positive effect on the formation of intestinal microflora. Breast milk contains hormones that promote intestinal maturation [7].
Recent studies indicate that there are differences in the content of immunological protection factors (in particular, secretory immunoglobulin (Ig) A) in the breast milk of women who gave birth at different stages of pregnancy (Table 1).
However, a number of studies indicate that breast milk does not fully meet the high needs of premature infants for energy and protein, a number of vitamins (fat-soluble - A, D, E, K and water-soluble - vitamin C, folic acid) and minerals (calcium, phosphorus, magnesium) [9].
Nevertheless, there is no doubt that human milk is the optimal nutrition for premature babies, therefore all efforts of medical personnel should be aimed at maintaining breastfeeding to the maximum extent possible, taking into account the special biological value of mother's native (freshly expressed) milk for a premature baby and the important role of mother-newborn contact during feeding.
It has been established that temperature treatment negatively affects the nutritional value of human milk: when feeding with pasteurized breast milk, the increase in body weight in the first month of life is insufficient and averages 9.6 ± 0.4 g/kg/day [10].
It has been proven that the milk of women who gave birth prematurely can satisfy the nutritional needs of premature children weighing more than 1700–2000 g. At the same time, premature children with a lower body weight after the end of the early neonatal period gradually begin to experience a deficiency in protein, calcium, phosphorus, magnesium, sodium, copper, zinc and vitamins B2, B6, C, D, E, K, folic acid and require nutrition optimization - enrichment of diets [11].
Feeding methods for premature babies
In maternity hospitals and neonatology departments, the following methods of feeding premature babies and their combinations are currently used.
- Parenteral nutrition - through central or peripheral veins (the feasibility of its combination with minimal enteral nutrition, which supports the functioning of the gastrointestinal tract (GIT) and stimulates its further maturation, has now been proven).
- Long-term tube feeding using infusion pumps (nasogastric tube).
- Portioned tube feeding (carried out using a syringe).
- Breastfeeding (true breastfeeding, feeding with expressed breast milk).
- Mixed or artificial feeding using special formulas for premature babies.
The figure shows the sequence of using feeding methods for premature infants.
Depending on the gestational age, body weight of the child and clinical status, premature infants in some cases require total parenteral nutrition. In order to maintain the peristaltic and secretory activity of the gastrointestinal tract, enteral nutrition is introduced gradually and in increasing volumes. Feeding is initially given through a tube and then gradually replaced by bottle feeding using breast milk or special formulas for premature babies.
For children weighing 1800–2000 g, a bottle feeding trial is performed. If sucking activity is unsatisfactory, tube feeding is carried out (usually using the portion method) in full or partial volume [10, 12].
Newborn babies weighing more than 2000 g with an Apgar score of 7 points or higher can be placed on the mother's breast in the first day of life. Typically, in a maternity hospital or hospital, a feeding regimen of 7–8 times a day is established. For premature babies, a free feeding regime is unacceptable due to their inability to regulate the volume of sucked milk and the high incidence of perinatal pathology, however, night feeding is possible. When breastfeeding, it is necessary to closely monitor the appearance of signs of fatigue - perioral and periorbital cyanosis, shortness of breath, etc. The presence of these symptoms is an indication for less frequent breastfeeding or for partial supplementary feeding with expressed milk from a bottle, or for a complete transition to bottle feeding [10 ].
Thus, the choice of feeding method should be strictly individual, determined by the degree of physiological maturity of the child, the clinical condition of the patient and accordingly change as it improves.
When calculating nutrition for premature babies, you should use only the “calorie” method, which involves the following calculation of nutrition [12] depending on the age of the child: 1st day - 30 kcal/kg; 2nd day - 40 kcal/kg; 3rd day - 50 kcal/kg; 4th day - 60 kcal/kg; 5th day - 80 kcal/kg; 6th day - 80 kcal/kg; 7th day - 90 kcal/kg; days 10–14 – 100–120 kcal/kg; Day 30 - 130 kcal/kg (artificial), 140 kcal/kg (breast milk).
As the child’s clinical condition improves and stable weight gain is established, as well as an active sucking reflex, the child is transferred to breastfeeding or fed expressed breast milk in combination with a special formula for premature babies.
Special formulas for premature babies
Clinical experience shows that most mothers experience hypogalactia after premature birth. The situation is aggravated by the fact that children have a reduced or absent sucking reflex, which further contributes to the extinction of lactation. In this regard, there is a need to use special formulas for premature babies. When developing them, the special needs of such infants for energy and nutrients are taken into account and, of course, the insufficient maturity of the digestive system is taken into account, which is a limiting factor in the absorption of a number of essential nutrients (lactose, fats, fat-soluble vitamins, etc.) [13].
The ratio of casein and whey proteins is close to that in breast milk; in modern formulas for premature babies it is 40:60.
Modern special mixtures (for example, Frisopre) that best meet the child's needs include nucleotides, which promote faster somatic growth and strengthen the immune system of children. Information on the content of nucleotides in breast and cow's milk, as well as European recommendations for their content in infant formula, adopted in 1996, are presented in Table 2.
In the body, nucleotides act as regulators of various biosynthesis processes. In turn, they can be synthesized in body tissues and (under normal conditions) are not essential nutrients. But this synthesis is energy-intensive and its volume is limited, as exemplified by the intense synthesis of nucleotides in the intestinal mucosa of newborns. Therefore, under certain conditions, especially during intensive growth, dietary nucleotides begin to acquire great importance [14].
Nucleotides have a positive effect on the maturation of intestinal epithelial cells and contribute to better formation of intestinal villi. By having a positive effect on the formation of intestinal microflora, nucleotides thereby improve the processes of absorption of nutrients. This leads to normalization of stool consistency and frequency [14].
The inclusion of glutamic acid and arginine in the Frisopre mixture activates the maturation processes of the intestinal mucosa and increases the efficiency of absorption of nutrients. Arginine is also added to the mixture in order to increase the biological value of the protein and additionally promotes the maturation of the immune system.
The amino acid tryptophan stimulates the production of serotonin, which, in turn, is necessary for brain development and is a precursor to the synthesis of melatonin, which regulates the change in circadian rhythms of sleep and wakefulness [15].
Taurine, a free amino acid not bound to protein, plays an important role in the development of nervous tissue and the brain. Taurine is necessary for the synthesis of new tissues and promotes active cell proliferation, which is especially important in the perinatal period. Taurine also takes part in the protection of cell membranes from exogenous toxins, participates in the formation of visual elements of the retina and in the synthesis of bile acids.
The fatty acid composition of formulas for premature infants is also extremely important, primarily due to the fact that they have limited endogenous synthesis of the most important long-chain polyunsaturated fatty acids - arachidonic and docosahexaenoic [16]. The latter are included in some products (Frisopre, Pre NAN, Humana 0-GA) and play a significant role in the structure and function of biological membranes and are essential components of brain phospholipids and photoreceptors of the retina [17].
The fat component of a number of products (Humana 0-HA, Pre-Nutrilak, Frisopre, Pre NAN) includes medium-chain triglycerides, which ensure the absorption of fat without the action of lipase, high absorption of fat in the intestines, and better absorption of calcium and zinc [16].
In the carbohydrate component, the lactose content is slightly reduced in order to avoid excess load on the gastrointestinal tract of low birth weight children (who are characterized by a limited ability to absorb milk sugar). In addition to lactose, a number of products (Humana 0-HA, Pre-Nutrilak, Pre NAN) contain a glucose polymer - dextrin-maltose, and some - polysaccharides in the composition of glucose syrup (Frisopre, Pre-Nutrilon) [16].
The energy value of formulas for premature babies is, as a rule, slightly higher and ranges from 75–80 kcal/100 ml, although some products are proposed to be used in two standard dilutions, while receiving either more or less concentrated nutrition (for example: Pre NAN, Enfamil, Frisolac Prematur).
An essential component of infant formula for premature babies is the vitamin-like substance L-carnitine, which is involved in the metabolism of fatty acids.
The introduction of dietary fiber (galactooligosaccharides) into the mixture provides good bifidogenic properties of the Frisopre product and promotes the growth of the child’s own bifidobacteria in the intestines, which is especially important for immature children, given the high frequency of dysbiotic disorders.
By the 17th day of life, energy needs increase to 130 kcal/kg/day. When artificial feeding, the caloric content of the diet should not exceed 130 kcal/kg/day. The use of human milk in the nutrition of premature infants, as well as mixed feeding, implies an increase in calorie content by the age of one month to 140 kcal/kg/day [12].
In the second month of life, the caloric content of a child’s diet depends on body weight at birth: in a child born with a body weight of more than 1500 g, the caloric content of the diet decreases monthly by 5 kcal/kg to the norms accepted for mature children and amounting to 115 kcal/kg. Reducing the calorie content of the diet of very premature infants (birth weight less than 1500 g) is carried out at a later date - after 3 months of age.
The introduction of a specialized product into a child’s diet should be carried out gradually, over 5–7 days, taking into account individual tolerance. Artificial feeding with such a mixture should be continued until the child reaches a weight of about 3000 g, after which the child is gradually (over 1 month) transferred to a standard formula. In the future, if necessary (severe prematurity, small weight gain), formula for premature babies can remain in the baby’s diet for several months in a small volume (1-2 feedings). In this case, it is mandatory to calculate diets not only by calorie content, but also by the content of essential nutrients (especially protein).
Literature
- Yatsyk G.V., Studenikin V.M., Skvortsova V.A. Feeding newborns: A guide to neonatology. M.: MIA, 1998. pp. 205-214.
- Tsang RC, Lucas A., Uauy R., Zlotkin S. Nutritional needs of the preterm infant//Caduceus. Medical. Publichers. Pawling. 1992.
- Sellmayer A., Kolezko B. Long-chain polyunsaturated fatty acids and eicosanoids in infants-physiological; and pathophysiological aspects and open questions//Lipids. 1999; 34 (2): 199-205.
- Gribakin S. G., Netrebenko O. K., Studenikin V. M., Skvortsova V. A. Principles of feeding premature newborns. M.: Soyuzmedinfo, 1989. 53 p.
- Skvortsova V. A., Borovik T. E., Lukoyanova O. L. et al. Current trends in the problem of feeding premature infants // Issues. modern pediatrics. 2005. No. 2. P. 80-86.
- Yatsyk G.V., Studenikin V.M. Feeding premature babies: Method. recommendations. M., 1997. 18 p.
- Volodin N.N., Mukhina Yu.G., Geraskina V.P., Chubarova A.I. Feeding premature babies. M., 2002. 46 p.
- Bulatova E. M. Feeding young children in modern conditions: Abstract of thesis. dis. ...Dr. med. Sci. St. Petersburg, 2005. 51 p.
- Lukoyanova O. L. Vitamin provision of premature infants in the neonatal period: Abstract of thesis. dis. ...cand. honey. Sci. M., 2000. 23 p.
- Feeding premature babies: A guide to therapeutic nutrition for children / ed. K. S. Ladodo. M.: Medicine, 2000. P. 101-111.
- Netrebenko O.K. Some essential micronutrients in the nutrition of premature infants. M., 2004. 136 p.
- Borovik T. E., Yatsyk G. V., Ladodo K. S., Skvortsova V. A. Rational feeding of premature infants (modern principles) // Issues of pediatric dietology. 2004. No. 6. P. 87-94.
- Shulman RJ, Schandler J., Lau C. et al. Early feeding, feeding tolerance and lactase activity in preterm infants//J. Pediatr. 1998; 133: 645-649.
- Schlimme E., Martin D. Nucleotid-supplementierung von Sauglingsnahrung. Kieler Milchwirtschaftliche Forschungsgerichte. 1999; 51 (3): 215-224.
- Guide to children's nutrition / ed. V. A. Tutelyan, I. Ya. Konya. M.: MIA, 2004. 568 p.
- Mukhina Yu. G., Chubarova A. I., Geraskina V. P. Macronutrients in the nutrition of premature infants // Children's Hospital. 2002. No. 2. P. 28-34.
- Uauy R., Hoffman DR Essential fat requirements of preterm infants//Am. J. Clin. Nutr. 2000; 71: 245-250.
V. A. Skvortsova, Doctor of Medical Sciences T. E. Borovik, Doctor of Medical Sciences, Professor G. V. Yatsyk, Doctor of Medical Sciences, Professor S. G. Gribakin, Doctor of Medical Sciences A. V. Andreeva O. L. Lukoyanova , Candidate of Medical Sciences T. R. Chumbadze NCZD, , Moscow
What formulas are best for a premature baby?
The goal of any composition for babies born prematurely is to gain muscle mass and catch up with their peers in development. Nutrition is prescribed by a pediatrician, taking into account the characteristics of a particular child. The doctor takes into account:
- baby's weight;
- general condition at the time of discharge from the maternity hospital;
- whether his mother partially breastfeeds (at least 1-2 times a day);
- Does the baby have allergies to food components?
Whether a brand is better or worse is determined separately in each case. A product suitable for 100 children may be useless for the 101st use.
The effectiveness and safety of the formula for an infant will be determined after several days of use. If an allergy or stool retention occurs, you should immediately notify your pediatrician. The doctor will choose a different brand.
How ratings are assigned
Manufacturers of formulas for premature and low birth weight babies test their developments in independent laboratories. These institutions are located either in the producing country or outside it. Then the manufacturers receive quality and safety certificates. These documents give the right to sell goods (mixtures) in specified countries or throughout the world.
Next, marketers come into play. They develop a sales strategy. Advertising occupies an important place in it. It determines the number of product purchases and ratings.
Popularity of brands:
- The rating of dairy formulations is headed by “Humana 0-VLB”. This is a liquid milk formula. It is ready for use. Contains live bacteria for normal intestinal function. Disadvantage: Sometimes babies suffer from constipation.
- Next, mothers prefer “Humana 0”. This is a dry formula for premature babies. It is perfectly absorbed by low-weight crumbs. Allergies occur very rarely.
- Nutrilon Pre 0 is often prescribed to low birth weight babies. The dry mixture has an enriched composition (calcium, iron, vitamins E). Disadvantage: Babies may experience constipation or colic.
- The dry mixture “Nutrilak Pre” is popular. It contains easily digestible proteins, probiotics, and folic acid. This is an excellent prevention of rickets.
- Doctors prescribe PreNan for babies who need to gain weight quickly. The product contains an increased amount of casein.
- Bellact Pre is ideal for babies with respiratory problems. It prevents diseases of the respiratory system.
- For accelerated and proper development of the nervous and digestive systems, pediatricians prescribe Friso Pre. The mixture is distinguished by a rich set of amino acids. But iron and zinc are available in insufficient quantities.
- For those who want to receive a complete replacement for breast milk, Hipp Pre is suitable. There is no sugar in the mixture. It does not give allergies. Babies don't have colic. But the product has low calorie content.
- For babies prone to allergies, Similak Neoshur is prescribed. The composition ensures rapid weight gain. Does not contain palm oil or sugar.
You will have to feed the baby for more than one day. Switching from one type to another is not always useful. When prescribing, the price category of the product should be taken into account.
Physical and psychomotor development of premature infants
Despite the progress achieved in their care, the physical development of very premature babies, even in the best perinatal centers, is significantly lower than the indicators characteristic of a healthy fetus in the corresponding intrauterine period. By the 28th day of life, the proportion of children whose weight is below the 10th centile corridor increases, according to CR Martin et al. (2009), from 18 to 75% [13]. According to our own data, the z-body mass index of premature infants born at 32 weeks and earlier decreases from 0.5 to 2 at the time of discharge [14]. In the first year of life, children can demonstrate “catch-up growth,” when the z-index of body weight and height approaches the norm: according to AC Westerberg et al. (2010), who studied the development of children with very low body weight, the z-index on average increases for it by 0.40, for height - by 1.01, but in general, premature children by the end of the first year of life have lower height and body weight than their full-term peers [15].
Data on the psychomotor development of preterm infants show that children, especially those born with very low and extremely low body weight, have worse developmental indicators than their full-term peers. According to BE Stephens et al., motor development scores on the Bayley scale below 70 points (which corresponds to low development) occur in 29% of premature infants, mental development in 22%, and the average motor and mental development score is 79. and 78 points, respectively [16].
Many researchers come to the conclusion that this developmental delay is primarily due to insufficient protein intake [17]. Thus, in the work of RJ Cooke and IC Griffin, it was established that while there was a general lag in physical development parameters by 37 weeks of gestation, the accumulation of fat mass in premature infants was higher, and lean mass was lower than in healthy children at the same time. The authors conclude that despite following current recommendations, children actually do not get enough protein. Moreover, the more fat, the more it accumulated in the waist area, which makes one think about the risk of metabolic syndrome in the future [18]. Protein deficiency is also considered the leading cause of delayed psychomotor development in premature infants. The longest-running study involving 424 infants receiving a standard adapted formula or a specialized preterm formula (with a higher protein content) showed that children in the second group had significantly higher rates of motor and mental development at both 18 months and 18 months of age. 7.5–8 and 16 years [19–22]. An increase in amino acid intake for each g/kg/day in the first week of life increases the motor development index of children by 8.2 points on the Bayley scale [16].
In addition to protein deficiency, low frequency of breastfeeding plays an important role in the delay in psychomotor development of premature infants. According to a study by A. Lucas et al., children who received breast milk, including donor milk (despite its lower protein content), had an intellectual development index (IQ) at early school age that was 8.3 points higher than those who received any artificial feeding. V. Bier et al. also studied the effects of breastfeeding on cognitive and motor development. They found that preterm infants who received breast milk at corrected ages of 3 and 12 months had significantly better motor and cognitive development scores. This work also revealed a direct relationship between the volume of milk received during hospitalization and the cognitive development of children at 7 and 12 months [23]. A meta-analysis conducted in 1998 showed that milk-fed children had 3.16 points higher cognitive development than formula-fed children. The effect was observed from 6 months to a minimum of 15 years. Longer duration of breastfeeding was associated with
large differences in cognitive development. Moreover, in children with normal birth weight, IQ was 2.66 points higher, while in children with low birth weight the difference was more significant - by 5.18 points. The results of this meta-analysis showed that for the most compromised groups of children, breastfeeding is more important than for healthy ones, i.e., the absence of breast milk in the diet has significantly more pronounced negative consequences [24]. Finally, the state of his mental sphere depends on feeding a child after birth. In the work already mentioned above by A. Lucas et al. Premature infants who received full-term formula had slightly worse socialization scores than those who received a specialized product. Moreover, evidence has emerged indicating that the frequency of neuroses and psychopathic conditions is higher in people who were bottle-fed.
One component of breast milk that may be responsible for better psychomotor development is long-chain polyunsaturated fatty acids (LCPUFAs). They, especially docosahexaenoic (DHA, 22:6 ω3), arachidonic (ARA, 20:4 ω6) and eicosapentaenoic (EPA, 22:5 ω3) acids, have many physiological effects, including participation in immune responses, inflammation, hemodynamic regulation , bone density. In premature infants, improvements in nervous system function with the use of DPFA have been reported in many studies. Thus, the benefits of using a formula enriched with DHA and ARA in premature infants born at more than 32 weeks of gestation in relation to motor and mental development by 6 months and 1 year were demonstrated in the work of PC Fang et al. (2005) [25]. The inclusion of γ-linolenic acid (as a precursor of ARA) and DHA in the diet of preterm infants resulted in improvements in IQ in boys compared with the unfortified formula, but no effect in the group as a whole. In the entire group receiving the study diet, an increase in the rate of increase in body weight and length from birth to the 9th month of life was detected, with a more pronounced effect also in boys [26]. A meta-analysis conducted in 2000 based on 9 studies available at that time showed the benefits of enriching the diet of premature infants with DPFA in relation to the development of visual function by the 2nd and 4th months of life [26]. The use of formulas containing DHA or ARA in preterm infants was associated with no changes in visual function at postconceptional ages 48 and 57 [27]. This study also noted a positive effect of the inclusion of DHA and ARA in the diet on the physical development of preterm infants: growth rates characteristic of full-term infants at the same postconceptional age were achieved.
In summary, despite the lack of evidence, due in part to the limitations of the techniques used, the inclusion of DHA and ARA in formula feeding may provide some benefits in terms of immune function, psychomotor and physical development. More pronounced positive effects are observed in children with a high risk of impairment of the tested functions. No studies have reported any side effects from the inclusion of these components in the diet of newborns.
In recent years, the attention of scientists has also been drawn to the carotenoid lutein, contained in breast milk in an amount of about 21 μg/l. It was found that in children receiving breast milk, the concentration of lutein in the serum is 6 times higher than in those receiving formula without this component [29]. To achieve similar serum concentrations, infants with formula should receive 4 times more lutein. A study of the effectiveness of a formula enriched with lutein in an amount of 200 μg/l, compared with a formula without lutein, but similar in other components, in full-term children did not reveal differences in their physical development [30]. The possible effects of lutein use in premature infants still require study.
The practice of feeding steadily gaining weight in premature and low birth weight infants
The above data suggest that preterm infants who have reached a postconceptional age of 37–40 weeks (i.e., the same age at conception as full-term infants) do not meet the physical and psychomotor development parameters of their full-term peers. Therefore, their diet cannot fully correspond to the usual diet of full-term infants. Such children need more calories, protein, food enrichment with a number of vitamins, immunonutrients, and minerals for quite a long time. At the same time, the protein content in their diet should be lower than in products for very premature infants, but higher than in breast milk.
When exclusively breastfed, the weight of children at 6 weeks of corrected age is 500 g less, their body length is 1.6 cm less than when fed with an enriched formula; the difference persists from 6 weeks to 9 months [20–23]. Therefore, for premature babies who are breastfed, fortification of breast milk is recommended.
When artificial feeding requires a special approach to the selection of nutrition. Longer-term use of preterm formula compared with standard adapted term formula has been shown to improve physical development outcomes. Feeding with formula for premature infants after discharge (up to the corrected age of 12 months) compared with formula for full-term infants leads to an increase in body weight at the age of 1 and 2 months, and an increase in height by 3 months. In children born with a body weight of less than 1250 g, feeding with a preterm formula is accompanied by a better effect in terms of increasing body length by 6 months and head circumference by 1, 3, 6 and 12 months [31].
However, for preterm infants, it appears that it is important to address more than just calorie and macronutrient issues. Long-term (up to a year) feeding of a formula enriched with calories, protein, calcium, and phosphorus had no advantages over standard full-term formula in terms of weight, height, and bone density in children born at 24–34 weeks [32].
Summarizing the data available by 2006, the nutrition committee of the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition Commite on Nutrition (ESPGAN) developed recommendations according to which:
1. Children born prematurely require careful monitoring of indicators of physical development, including height, head circumference, body composition; 2. When artificial feeding, a standard formula enriched with DPFA is recommended; 3. Children discharged with reduced weight and height for a given postconceptional age should receive fortified breast milk or a specialized formula fortified with protein, minerals and trace elements until at least the 40th week of postconceptional age, and possibly until the 52nd week weeks [33].
In the opinion of the authors, in Russia insufficient attention is paid to careful monitoring of the physical development of premature infants and, no less important, to its correct assessment using modern scales of physical development. It is obvious that by the time of transition to exclusively enteral nutrition and in the period of preparation for discharge, children need differentiated nutritional prescriptions depending on physical development and nutrition correction in case of a decrease in physical development parameters. Children with weight and especially length below the 25th centile need to be fed foods high in protein and calories. Children whose development corresponds to the average for their age in the period of preparation for discharge (on reaching a body weight of 1800 g or more) no longer need such high levels of protein and calorie intake as very premature children, but at the same time, all children need in obtaining a number of regulatory nutrients, such as DPFA, nucleotides, lutein, growth factors, etc.
Therefore, the registration in Russia of specialized food products intended for feeding premature and low birth weight infants in the intermediate period between the end of intensive nutritional support (usually upon reaching a body weight of 1800 g or more) and approaching developmental indicators corresponding to full-term infants should be assessed as a positive trend. This is the so-called subsequent mixtures. Such a product is, in particular, the Similac Neosure mixture (Abbott Nutrition), which provides a child’s protein intake at the level of 3 g/kg with a food intake of 160 ml/kg and 3.2 g/kg with a food intake of 180 ml/kg per day . The mixture contains ARA and DHA in amounts of 0.1 and 0.4% (16 and 6 mg per 100 ml), respectively, of the total fatty acid content. The mixture contains growth factors and nucleotides. A special feature of the product is its high lutein content. The mixture can already be used by children with a body weight of 1800 g, provided that the parameters of their physical development correspond to the 25th centile or more corridor for a given post-conceptual age. It is advisable to start using the product in a hospital to ensure careful control over physical and psychomotor development. After discharge, the formula can be recommended for feeding for at least 40 weeks for children who are not lagging behind in physical development, and for children with postnatal delay in physical development - up to 56 weeks. The feasibility of longer-term use of such products is being studied.
Literature
1. Waterland RA, Michels KB Epigenetic epidemiology of the developmental origins hypothesis. Annu Rev Nutr 2007;27:363–88. 2. Labayen I, Moreno LA, Ruiz JR, et al. Avena Study Group Small birth weight and later body composition and fat distribution in adolescents: the Avena study Obesity (Silver Spring) 2008;16(7):1680–86. 3. Ruiz JR, Labayen I, Ortega FB. Birth weight and blood lipid levels in Spanish adolescents: Influence of selected APOE, APOC3 and PPARgamma2 gene polymorphisms. 4. Yajnik CN, Fall CH, Coyaji KJ. Neonatal anthropometry: the thin-fat Indian baby. The pune mar- ternal nutrition study. Int J Obes Rel Metab Disord 2003;27:173–80. 5. Joglekar CV, Fall CH, Deshpande VU, et al. Newborn size, infant and childhood growth, and body composition and cardiovascular disease risk factors at the age of 6 years. The pune maternal nutrition study Int J Obes (Lond) 2007;31(10):1534–44. 6. Harder T, Rodekamp E, Schellong K, et al. Birth weight and subsequent risk of type 2 diabetes: a meta-analysis. Am J Epidemiol 2007;165(8):849–57. 7. Barker DJ, Osmond C, Simmonds SJ, et al. The relation of small head circumference and thinness at birth to death from cardiovascular disease in adult life. Br Med J 1993;306:422–26. 8. Huxley R, Neil A, Collins R. Unravelling the fetal origins hypothesis: there is really an inverse association between birthweight and subsequent blood pressure. Lancet 2002; 360:659–65. 9. Raikkonen K, Pesonen AK, Heinonen K, et al. Depression in young adults with very low birth weight: the Helsinki study of very low-birth-weight adults. Arch Gen Psychiatry 2008;65(3):290–96. 10. Cauderay M, Schutz Y, Micheli JL, et al. Energy-nitrogen balances and protein turnover in small and appropriate for gestational age low birthweight infants. Eur J Clin Nutr 1988;42(2):125–36. 11. Embleton NE, Pang N, Cooke RJ Postnatal malnutrition and growth retardation: an inevitable consequence of current recommendations in preterm infants? Pediatrics 2001;107(2):270–73. 12. Bruin NC, Degenhart HJ, Gal S, et al. Energy utilization and growth in breast-fed and formulafed infants measured prospectively during the first year of life. Am J Clin Nutr 1998; 67(5):885–96. 13. Martin CR, Brown YF, Ehrenkranz RA, et al. Nutritional practices and growth velocity in the first month of life in extremely premature infants. Pediatrics 2009;124(2):649–55. 14. Dorofeeva A.B., Glupanova E.V., Getia E.G. and others. Physical development of premature newborns in a hospital setting. Materials of the IX Russian Congress “Innovative technologies in pediatrics and pediatric surgery” 10/19–22/2010. pp. 217–18. 15. Westerberg AC, Henriksen C, Ellingvag A, et al. First year growth among very low birth weight infants. Acta Paediatr 2010;99(4):556–62. 16. Stephens BE, Walden RV, Gargus RA, et al. Firstweek protein and energy intakes are associated with 18-month developmental outcomes in extremely low birth weight infants. Pediatrics 2009;123(5):1337–43. 17. Arslanoglu S, Moro GE, Ziegler EE. Preterm infants fed fortified human milk receive less protein than they need. J Perinatol 2009;29(7):489–99. 18. Cooke RJ, Griffin I. Altered body composition in preterm infants at hospital discharge. Acta Paediatr 2009;98(8):1269–73. 19. Lucas A, Morley R, Cole TJ, et al. Early diet in preterm babies and developmental status at 18 months. Lancet 1990;335(8704):1477–81. 20. Lucas A, Morley R, Cole TJ, et al. Breast milk and subsequent intelligence quotient in children born preterm. Lancet 1992;339(8788):261–64. 21. Lucas A, Morley R, Cole TJ. A randomized multicentre study of human milk versus formula and later development in preterm infants. Arch Dis Child 1994;70:141–46. 22. Morley R, Lucas A. Randomized diet in the neonatal period and growth performance until 7.5–8 y of age in preterm children. Am J Clin Nut 1998;3:822–28. 23. Bier BJA, Oliver T, Ferguson AE, et al. Human milk improves cognitive and motor development of premature infants during infancy. J Hum Lact 2002;18:361–67. 24. Anderson JW, Johnstone BM, Remley DT. Breastfeeding and cognitive development: a metaanalysis. Am J Clin Nutr 1999;70:525–35. 25. Fang PC, Kuo HK, Huang CB, et al. The effect of supplementation of docosahexaenoic acid and arachidonic acid on visual acuity and neurodevelopment in larger preterm infants. Chang Gung Med J 2005;28(10):708–15. 26. Fewtrell MS, Abbott RA, Kennedy K, et al. Randomized, double-blind trial of long-chain polyunsaturated fatty acid supplementation with fish oil and borage oil in preterm infants. J Pediatr 2004;144(4):471–79. 27. SanGiovanni JP, Parra-Cabrera S, Colditz GA, et al. Meta-analysis of dietary essential fatty acids and long-chain polyunsaturated fatty acids as they relate to visual resolution acuity in healthy preterm infants. Pediatrics 2000; 105:1292–98. 28. Innis SM, Adamkin DH, Hall RT, et al. Docosahexaenoic acid and arachidonic acid enhance growth with no adverse effects in preterm infants fed formula. J Pediatr 2002;140(5):547–54. 29. Bettler J, Zimmer JP, Neuringer M, et al. Serum lutein concentrations in healthy term infants fed human milk or infant formula with lutein. Eur J Nutr 2010;49(1):45–51. 30. Capeding R, Gepanayao CP, Calimon N. Luteinfortified infant formula fed to healthy term infants: evaluation of growth effects and safety Nutr J 2010;9:22. 31. Carver JD, Wu PYK, Hall TR. Growth of Preterm Infants Fed Nutrient-Enriched or Term Formula After Hospital Discharge. Pediatrics 2001;107;683–89. 32. Koo WW, Hockman EM. Posthospital discharge feeding for preterm infants: effects of standard compared with enriched milk formula on growth, bone mass, and body composition. Am J Clin Nutr 2006;84(6):1357–64. 33. Aggett PJ, Agostoni C, Axelsson I, et al. Society for Pediatric Gastroenterology, Hepatology, and Nutrition Commite on Nutrition. Infants after hospital Discharge J Ped Gastr Nutr 2006;42:596–603.
About the authors / For correspondence
Chubarova Antonina Igorevna – Doctor of Medical Sciences, pediatrician, neonatologist, professor of the Department of Hospital Pediatrics of the Pediatric Faculty of the Russian Research Medical University. N.I. Pirogov. Tel., e-mail; Yulia Grigorievna Mukhina – Doctor of Medical Sciences, Professor, pediatrician, gastroenterologist, Head of the Department of Hospital Pediatrics, Pediatric Faculty, Russian Research Medical University. N.I. Pirogov. Tel.; Dorofeeva Anna Borisovna – pediatrician, graduate student of the Department of Hospital Pediatrics, Pediatric Faculty, Russian Research Medical University. N.I. Pirogov. Tel.
Similar articles
- Functional gastrointestinal disorders in children: treatment algorithms
- The importance of polyunsaturated fatty acids in complex acne therapy
- Nutritional deficiency, its causes and ways of correction in children with central nervous system tumors during the stage of active therapy and after its completion
- Clinical experience with the use of the drug Vitrum Cardio Omega-3 in the correction of metabolic disorders in women with early menopause
- Modern approaches to organizing nutrition for pregnant and lactating women in the Far North