Key Facts
- According to the Convention on the Rights of the Child, every child of infant and other age groups has the right to adequate nutrition.
- Malnutrition is associated with 45% of deaths among children.
- In 2013, an estimated 161.5 million children under five years of age were stunted worldwide and 50.8 million children had low weight-for-height, mainly as a consequence of poor feeding or repeated infections, while while 41.7 million children were overweight or obese.
- About 36% of children under 6 months of age are exclusively breastfed.
- Few children receive adequate, nutritious and safe complementary foods; In many countries, only one third of breastfed children aged 6–23 months receive complementary foods that meet age-appropriate dietary diversity and feeding frequency criteria.
- More than 800,000 children under 5 years of age could be saved each year through optimal breastfeeding of all children from birth to 23 months. Breastfeeding increases IQ, improves school attendance, and is associated with higher income in adulthood.
- Improving child development and reducing health care costs through breastfeeding leads to economic benefits both for individual families and at the national level.
Review
It is estimated that malnutrition causes 3.1 million child deaths each year, or 45% of all child deaths.
Infant and young child feeding is an important strategy for improving child survival and promoting healthy growth and development. The first two years of a child's life are especially important, as optimal nutrition during this period helps reduce morbidity and mortality, reduce the risk of chronic diseases and improve overall development. Optimal breastfeeding is critical and could save more than 800,000 children under 5 years of age every year. In countries with high rates of child stunting, promoting breastfeeding and adequate complementary feeding could prevent approximately 220,000 deaths among children under 5 years of age. WHO and UNICEF recommendations for optimal infant and young child feeding are as follows:
- early initiation of breastfeeding within an hour after the birth of the baby;
- exclusive breastfeeding for the first six months of life;
- Introducing appropriate, nutritious and safe complementary foods at six months of age, with continued breastfeeding until the child is two years of age or older.
However, many infants and other age groups do not receive optimal nutrition; for example, on average, only 36% of children under 6 months of age are exclusively breastfed.
Recommendations have been updated to meet the needs of infants born to HIV-infected mothers. Now, thanks to antiretroviral drugs, these children can be exclusively breastfed for up to six months and continue to be breastfed for at least 12 months, with a significant reduction in the risk of HIV transmission.
Breastfeeding is one of the most effective ways to ensure the health and survival of children. Through optimal breastfeeding and complementary feeding, malnutrition can be avoided and approximately one million children's lives can be saved each year. Worldwide, less than 40% of infants under six months of age are exclusively fed breast milk. By providing mothers and families with adequate support to breastfeed, many children's lives could be saved.
WHO actively promotes breastfeeding as the best source of nutrition for infants and young children. This fact sheet explores the many positive aspects of the practice and how breastfeeding can be increased around the world through active support for mothers.
1. WHO strongly recommends exclusive breastfeeding for the first six months of life. From six months of age, other foods should supplement mother's milk until age two or more. In addition: breastfeeding should begin within an hour of birth; Breastfeeding should be done “on demand” as often as the baby wishes, day and night, and the use of bottles or nipples should be avoided.
2. Beneficial effect on children's health.
Breast milk is the ideal nutrition for newborns and infants. It contains all the nutrients necessary for the healthy development of babies. It is safe and contains antibodies that help protect babies from common childhood illnesses such as diarrhea and pneumonia, two leading causes of child mortality worldwide. Mother's milk is always available and affordable, which helps ensure adequate nutrition for babies.
3. Breastfeeding is also beneficial for mothers.
The practice of exclusive breastfeeding is associated with a natural (but not guaranteed) way to prevent pregnancy (98% protection in the first 6 months after birth). Breastfeeding reduces the risk of developing breast and ovarian cancer later in life, helps women return to their pre-pregnancy weight more quickly, and reduces rates of obesity.
4. Long-term benefits for children.
In addition to the immediate benefits for children, breastfeeding promotes good health throughout life. Adults who were breastfed as infants often have lower blood pressure and cholesterol levels, as well as lower rates of overweight, obesity and type 2 diabetes. There is evidence that breastfed individuals perform better on intelligence tests.
5. Why it is not advisable to use infant formula.
Powdered infant formula does not contain the antibodies found in breast milk. If infant formula is not prepared properly, there are a number of dangers associated with the use of unsafe water and unsterilized equipment, or the potential presence of bacteria in the powdered formula. Excessive dilution of the formula with water in order to “stretch” reserves can lead to malnutrition. In addition, frequent breastfeeding helps maintain an adequate supply of breast milk. If the formula being used becomes unavailable and the mother returns to breastfeeding, breast milk production may decrease.
6. HIV and breastfeeding.
An HIV-infected mother can pass the infection to her baby during pregnancy, childbirth, and breastfeeding. Antiretroviral drugs (ARVs) given to a mother or child exposed to HIV help reduce the risk of HIV transmission during breastfeeding. Breastfeeding combined with ARVs has the potential to significantly improve a child's chances of survival by preventing HIV infection. According to WHO recommendations, HIV-infected mothers during breastfeeding should receive ARVs and follow WHO guidelines regarding breastfeeding and complementary feeding.
7. Regulation of breast milk substitutes.
The International Code of Marketing of Breast-milk Substitutes was approved in 1981. It provides:
· all labels and all information must contain instructions about the benefits of breastfeeding and the health risks of substitutes;
· ban on advertising of breast milk substitutes;
· a ban on the distribution of free samples of substitutes to pregnant women, mothers or their families;
·prohibition of the distribution of free or subsidized substitutes to health care workers or in health care facilities.
8. Providing support to mothers.
Breastfeeding takes a learning curve, and many women struggle at first. Often there is pain in the nipples and concerns about the lack of milk for long-term feeding of the child. Health facilities that support breastfeeding by providing trained breastfeeding educators to help new mothers help increase breastfeeding rates. Today, thanks to the WHO-UNICEF initiative, more than 20,000 facilities in 152 countries operate to provide this support and improve maternal and newborn health care.
9. Work and breastfeeding.
Many mothers returning to work give up breastfeeding partially or completely because they do not have the time or adequate space to breastfeed, express and store their milk. To continue breastfeeding, mothers must have access to safe, clean, designated areas at work or nearby. This can be achieved by creating supportive work environments such as paid maternity leave, part-time work, on-site nurseries, facilities for expressing and storing breast milk and breastfeeding breaks.
10. Next step: gradual inclusion of new foods in the diet.
To meet the growing needs of infants six months and older, additional foods must be introduced into the diet while breastfeeding continues. WHO notes that:
·When starting additional feeding, you should not reduce breastfeeding;
·complementary foods should be given from a spoon or cup rather than in a bottle;
·food must be clean, safe and locally available;
· Sufficient time is required for children to learn to eat solid foods.
Until what age each mother decides to feed her baby herself.
At the same time , introducing complementary foods does not guarantee complete absorption of the products.
With their help, the baby gets acquainted with new tastes and textures. The benefits of feeding up to two years include good weight gain in children. Such babies are stronger and more resilient, and they are less likely to have health problems. GBUZ "Center for Medical Prevention" of the Ministry of Health of the Krasnodar Territory.
Breast-feeding
Exclusive breastfeeding for six months has many benefits for infants and their mothers. The main ones are protection against gastrointestinal infections, observed not only in developing but also in industrialized countries. Early initiation of breastfeeding—within an hour of birth—protects the newborn from infections and reduces neonatal mortality. The risk of death from diarrhea and other infections may be higher among children who were previously partially breastfed or not breastfed at all.
Breast milk is also an important source of energy and nutrients for children aged 6-23 months. It can provide half or more of a baby's energy needs between 6 and 12 months and one-third of a baby's energy needs between 12 and 24 months. Breast milk is also an important source of energy and nutrients during illness and helps reduce mortality among malnourished children.
Children and adolescents who were breastfed as infants are less likely to be overweight or obese. They also show higher scores on intelligence tests and better school attendance. Breastfeeding is associated with higher income in adulthood. Improving child development and reducing health care costs through breastfeeding leads to economic benefits both for individual families and at the national level.
Longer breastfeeding also improves maternal health and well-being; it reduces the risk of ovarian and breast cancer and allows time between pregnancies - exclusive breastfeeding for children under six months of age has hormonal effects that often cause missed periods. This is a natural (though unreliable) method of preventing pregnancy, known as the lactational amenorrhea method.
Mothers and families need to be supported to ensure optimal breastfeeding for their children. Actions to protect, promote and support breastfeeding include:
- adopting policies such as the International Labor Organization Maternity Protection Convention No. 183 and Recommendation No. 191, which complement Convention No. 183 by offering longer leave and greater benefits;
- International Code of Marketing of Breast-milk Substitutes and subsequent relevant World Health Assembly resolutions;
- Implementing the Ten Principles for Successful Breastfeeding outlined in the Breastfeeding Friendly Hospital Initiative, including: providing skin-to-skin contact between mother and baby immediately after birth and initiating breastfeeding within the first hour of life child;
- breastfeeding on demand (that is, as often as the baby wants, day and night);
- Room sharing (allowing mothers and infants to be together 24 hours a day);
- Children should not be given additional food or drink, not even water.
Breastfeeding uptake is greatly facilitated by supportive interventions, and rates of exclusive and long-term breastfeeding can be improved within a few years.
Breastfeeding: WHO recommendations and other useful tips
Undoubtedly, for infants, especially in the first months, the ideal food is mother's milk. It not only contains all the necessary nutrients, enzymes, hormones, protective factors, but is also easily digested and absorbed by the baby’s body. So it is very important to maintain breastfeeding for as long as possible. The “Global Strategy” for breastfeeding was jointly developed by WHO and UNICEF. Below are its basic principles.
- Early breastfeeding - within the first hour after birth!
- Avoid feeding the newborn with a bottle or other method before the mother attaches him to the breast. This is necessary so that the child does not develop a mindset for any other feeding than breastfeeding.
- Joint maintenance of mother and child in the maternity hospital in the same ward.
- Correct positioning of the baby at the breast allows the mother to avoid many problems and complications with the breast. If the mother was not taught this in the maternity hospital, she should invite a lactation consultant and learn this specifically.
- Feeding on baby's demand. It is necessary to put the baby to the breast for any reason, to give him the opportunity to suckle when he wants and as much as he wants. This is important not only for satiating the child, but also for his psycho-emotional comfort. To feel comfortable, the baby can be attached to the breast up to 4 times per hour.
- The duration of feeding is regulated by the child: do not take the baby off the breast before he releases the nipple!
- Night feedings of the baby ensure stable lactation and will protect the woman from the next pregnancy for up to 6 months - in 96% of cases. In addition, it is night feedings that are the most complete and nutritious.
- No additional soldering or introduction of any foreign liquids and products. If the baby is thirsty, he should be put to the breast more often.
- Complete refusal of pacifiers, pacifiers and bottle feeding. If it is necessary to introduce complementary foods, it should be given only from a cup, spoon or pipette.
- Transferring the baby to the second breast only when he has suckled the first breast. If the mother rushes to offer the baby the second breast, he will not receive additional “late milk” rich in fats. As a result, the baby may experience digestive problems: lactose intolerance, foamy stools. Prolonged sucking on one breast will ensure proper bowel function.
- Avoid washing nipples before and after feeding. Frequent breast washing leads to the removal of the protective layer of fat from the areola and nipple, which leads to the formation of cracks. Breasts should be washed no more than once a day during a hygienic shower. If a woman showers less often, then in this case there is no need for additional breast washing.
- Refusal from control weighings of the child, carried out more than once a week. This procedure does not provide objective information about the nutritional status of the infant. It only irritates the mother, leads to a decrease in lactation and the unreasonable introduction of supplementary feeding.
- Elimination of additional milk expression. With properly organized breastfeeding, milk is produced exactly as much as the baby needs, so there is no need to pump after each feeding. Pumping is necessary in case of forced separation of mother and child, mother going to work, etc.
- Only breastfeeding up to 6 months - the child does not need additional nutrition or complementary foods. According to some studies, a child can be exclusively breastfed for up to 1 year without harming his health.
- Support for mothers who breastfed children up to 1-2 years of age. Communicating with women who have had positive experiences with breastfeeding helps a new mother gain confidence in her abilities and receive practical advice to help establish breastfeeding. Therefore, new mothers are advised to contact maternal breastfeeding support groups as early as possible.
- Training in child care and breastfeeding techniques is necessary for a modern mother so that she can raise him up to 1 year without unnecessary hassle and comfort for herself and her baby. Lactation consultants will help you arrange care for your newborn and teach your mother breastfeeding techniques. The sooner a mother learns motherhood, the fewer disappointments and unpleasant moments she and her baby will endure.
- Breastfeeding until the child is 1.5-2 years old. Breastfeeding for up to one year is not a physiological period for cessation of lactation, so both mother and child suffer during weaning.
RULE OF “DUTY CHEST”
One of the basic rules for successful breastfeeding is the “breast on duty” principle. A fairly common problem that young mothers face is that the baby does not completely empty the breast and does not receive enough “hind”, fatty and nutritious milk, but receives an excess of fore milk – “liquid” and sweet, with a high lactose content. As a result, problems with the gastrointestinal tract may arise, because the baby’s stomach is not able to independently digest a large volume of lactose, and the baby’s body would have to receive the enzymes necessary for its digestion with a portion of hind milk. Such unsystematic breastfeeding is also fraught with a decrease in lactation, because the mother’s body adapts to the child’s requirements - and if the child sucks the breast little by little and does not empty it, then less and less milk will be produced over time.
In this case, the “breast on duty” method will help. The bottom line is that, regardless of the number of attachments, only one breast is offered for 2-2.5 hours, then, for the next 2-2.5 hours, only the other. The rule of the duty breast is of particular importance during the establishment of breastfeeding, when the baby is latched on demand. In addition, this method significantly reduces the risk of milk stagnation. In addition, such periods of increased feeding frequency can occur in a child not only immediately after birth, but also in children with an already formed feeding interval during illness and during a lactation crisis in the mother (at 3-3.5 months, 6-7 months ).
Breastfeeding support website
Lure
At about six months of age, the baby's energy and nutritional needs begin to exceed the level at which they can be met by breast milk, and the introduction of complementary feeding becomes necessary. At this age, the child is ready to eat other foods and is developmentally ready. Not introducing complementary foods after the baby reaches six months of age or inappropriately introducing complementary foods can affect the baby's growth. The guidelines for proper complementary feeding are as follows:
- continue frequent, on-demand breastfeeding until the child is two years of age or older;
- Be sensitive when feeding your baby (for example, directly feed infants and assist older children. Feed slowly and patiently, encourage but not force, talk to your baby and maintain eye contact);
- practice good hygiene and proper food handling;
- Start at six months with small amounts of foods and gradually increase as the baby gets older;
- gradually increase the consistency of food and make it more varied;
- Increase the number of times your baby feeds - 2-3 times a day for children aged 6-8 months and 3-4 times a day for children aged 9-23 months, with 1-2 additional snacks as desired;
- Use fortified foods or vitamin and mineral supplements for complementary feeding as needed;
- increase fluid intake, including through breastfeeding, and offer soft, favorite foods.
Feeding under extremely difficult conditions
Families and children in difficult circumstances require special attention and practical support. Whenever possible, mothers and infants should remain together and receive the support they need to provide the most appropriate feeding in the given environment. Breastfeeding remains the preferred feeding option for babies in almost all difficult situations, such as:
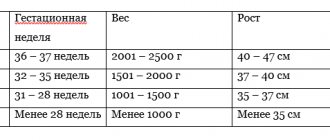
- low birth weight or premature babies;
- HIV-infected mothers;
- teenage mothers;
- malnourished infants and young children;
- families suffering from the consequences of complex emergencies.
HIV and infant feeding
Breastfeeding, especially early and exclusive breastfeeding, is one of the most effective ways to improve infant survival rates. However, HIV can be transmitted from mother to child during pregnancy, childbirth, and through breast milk. In the past, the challenge has been to balance the risk of infants acquiring HIV during breastfeeding with the increased risk of death from causes other than HIV, particularly from malnutrition and serious illnesses such as diarrhea and pneumonia, for uninfected infants who are not breastfed.
Evidence on HIV and infant feeding suggests that antiretroviral drugs (ARVs) given to an HIV-infected mother can significantly reduce the risk of HIV transmission through breastfeeding and also improve her health. This allows HIV-infected mothers to breastfeed their babies with a low risk of transmission (1-2%). Therefore, HIV-infected mothers and their infants living in countries where diarrhea, pneumonia and malnutrition are still common causes of death in infants and children can receive the benefits of breastfeeding with minimal risk of HIV transmission.
Since 2010, WHO has recommended that HIV-infected mothers take ARVs and exclusively breastfeed their babies for the first six months, followed by adequate complementary feeding and continued breastfeeding until their babies' first birthday. Breastfeeding should only be discontinued when a safe diet containing adequate nutrients can be provided without it.
Even if ARVs are not available, mothers should be encouraged to exclusively breastfeed for the first six months of their children's lives and continue until environmental and social conditions are safe and conducive to feeding infant formula.
Nutrition for a nursing mother
“What can I eat when I breastfeed?”
This is one of the few questions that worries almost every woman almost from the first weeks of pregnancy.
The expectant mother begins to search for information on the Internet or ask more experienced mothers. And at some point he realizes with surprise that if you collect all the found “diets for nursing mothers” and the advice of friends on this topic, it turns out that you can only drink water, boiled potatoes and tea with cow’s milk “to increase the amount of milk.” Agree, the prospect is bleak. Is that really true? Not only does the mother of a newborn need to adapt to a new and completely unfamiliar life with a little person, but she will also have to give up her favorite dishes? Let's figure it out.
What is breast milk?
To understand the mechanism of the influence of maternal nutrition on the composition of milk, we first find out how and from what milk is obtained.
So, milk is produced by special cells, lactocytes, which seem to line the surface of the alveoli - small “bags” that store milk inside the breast.
So, milk is produced by lactocytes from blood plasma components. And this is a key point, because it becomes clear that mother’s nutrition affects the composition of milk to approximately the same extent as the composition of blood. For example, the source of the formation of lactose (the main carbohydrate of milk) is predominantly circulating blood glucose, etc.
During the digestion process, the food eaten is broken down in the gastrointestinal tract and absorbed into the blood in the form of molecules and elements (not pieces of cabbage or cutlets :-)). Together with the blood, the molecules can enter the capillaries of the mammary gland, and from there into the milk through lactocytes (or they may not, this depends on many factors).
What can a nursing mother eat?
So what about the diet? The good news is that there is no such thing as a breastfeeding diet! This explains the scattered and often contradictory information on this topic in different sources. That is, there is no product that is guaranteed to lead to negative reactions in any child. There is a small list of products that, according to the observations of mothers and doctors, most often cause allergic reactions. BUT! This does not mean that these foods should be excluded from your diet completely. With a high degree of probability, they may not affect your baby’s well-being.
The basic rule for any new product is: “A little bit at a time.” Next, we watch the baby’s reaction and, in its absence, feel free to introduce the product into the usual diet. But even if there is a reaction, it most likely will not last forever. The baby’s gastrointestinal tract matures and functions better every month. Try the product to which you had a reaction again after 1.5-2 months. It is very possible that then the child will calmly accept it.
1. A certain amount of foreign protein enters the blood and, accordingly, into mother’s milk. In children of the first year of life, one of the main allergens that cause the development of food allergies is cow's milk protein. It is known that among children in the first year of life, an allergy to cow's milk proteins (CMP) occurs in 0.5–1.5% of breast-fed infants, and up to 2–5% in bottle-fed infants (most nutritional formulas are made based on cow's milk). In patients with atopic dermatitis, an allergy to CMP is detected in 70–85% of cases.
This sounds revolutionary against the backdrop of almost the most popular advice to drink tea with milk “for milk.” However, cow's milk protein is the world leader among children's allergens. Any foreign protein (and BKM is a native protein for a calf, and not for a human baby) is a very strong allergen. And if you count how much milk and milk-based products we consume daily, everything falls into place.
...I wonder, does a cow know that in order for her to produce more milk, she needs to drink the milk of other mammals? 
2. Another plant protein that often causes allergic reactions is gluten. Contained in most cereals. Gluten is absent in rice, buckwheat, millet (not to be confused with wheat, it contains it!) and corn.
This is, of course, no reason to deny yourself flour and longingly dream about your favorite spaghetti or morning sandwich. This information is needed in order to check this group of products if an allergy is suspected.
3. Dyes, preservatives, chemical additives, etc. Many of these components penetrate into the blood and, consequently, into milk. Well, everything is clear here. The human body of any age is not designed to ingest such substances. But if the gastrointestinal tract of an adult has somehow adapted and copes with this “chemical attack,” then for the digestive system of a newborn this may be an unbearable burden.
4. Brightly colored and citrus fruits and vegetables. Just like dyes and preservatives, they are most often either histamine liberators or cause worsening of the condition only as long as the true allergen is present in the diet. For example, a child has allergies. The mother excludes brightly colored fruits and vegetables from the diet, and the child’s condition improves slightly. The mother removes all dairy products from the diet, and the child recovers. The mother reintroduces bright fruits and vegetables into the diet - and the child tolerates them well. That is, the principle is the same: we ate 2 strawberries - we monitor the child’s reaction, etc.
5. Exotic dishes. Any products that are unusual or exotic for your family. If you really want to try some “overseas fruit”, try it for your health! Just a tiny piece. And watch the baby's reaction.
6. In the first months, it is worth limiting foods to which one of your family members is allergic. You can also try such products a little at a time and monitor the reaction.
7. Some other foods that, according to observations, cause an allergic reaction more often than others (!!! this does not mean that you should not eat them, it means that they should not be abused and that you also need to pay attention to them first of all when occurrence of allergies!!!). Eggs, seafood, soy, peanuts, tree nuts.
Diet for a nursing mother: official recommendations
And here is the recommended average daily set of food products for lactating women (g, gross), given in the “National Program for Optimizing the Feeding of Children in the First Year of Life” (Moscow, 2019). As you can see, modern official medicine also does not recommend a strictly restrictive diet for a nursing mother.
Here are some more common questions about nutrition while breastfeeding.
Question: Is it true that foods that cause increased gas formation in the mother (cabbage, peas, etc.) will also cause it in the child?
Answer: No, it's not true. Increased gas formation in a mother is an individual reaction of the mother’s body to a certain product. Gases are formed in the gastrointestinal tract and do not enter the blood, and, consequently, into the milk. However, during the digestion process, foreign proteins and other components enter the bloodstream, and the child may react to some of them. It is impossible to reliably predict this: each organism is individual. If you have doubts about a product, introduce it into your diet a little at a time, monitoring your baby’s reaction.
!!! It is also important to know that not all lactose (the main carbohydrate in breast milk) is broken down in the baby’s small intestine (and this is the NORMAL for breastfed babies). Undigested lactose moves further and stimulates the formation of beneficial intestinal colonies of Lactobacillus bifidus bacteria. These fermenting bacteria provide an acidic environment in the gastrointestinal tract and suppress pathogenic bacteria, fungi and parasites. Gases are a by-product of fermentation. An abundance of gas in infants in the first months of life is the norm!
Question: “I eat almost nothing but water and potatoes, but the child is still covered in acne. Is he allergic to my milk?
Answer: Breast milk is a natural and physiological product for the baby’s digestive system. If a baby has a reaction, it is usually caused by a foreign protein mixed into the mother's milk and not by components of the milk. It also often happens that when a mother begins to play it safe and severely limit her diet, the child’s condition worsens! This may be due to the fact that a stable, meager diet leads to the depletion of the resources of the mother’s body and the child begins to receive less of certain components and receive others in excess. The optimal solution in such a situation would be not a standard restrictive diet, but a search and identification of foods that are allergens specifically for your child. Well, it is important to know that in a child’s first months of life, changes in the skin are not always caused by allergic reactions. This may be a manifestation of certain physiological conditions. Consult your doctor. If the allergic nature of the rash is confirmed, you need to understand that the allergy can also be of a non-food nature (children's cosmetics, laundry detergents, pets or plants, etc.).
Question: Is it true that to have a lot of milk, you need to drink a lot? What if you don’t want to?
Answer: The secret is very simple: ANY warm drink helps increase the level of oxytocin, the hormone that causes milk to flow. If the mother drinks when thirsty, drinks a few sips (as much as she wants) of her favorite warm drink immediately before or during feeding, then the milk flows out more easily and more intensely. It doesn’t get bigger, it just flows out of the chest more easily! Drinking too much, in excess of thirst, can provoke swelling (including in the breast tissue), which can, on the contrary, impede the outflow of milk and provoke stagnation.
Question: I have to eat a lot so that my baby gets enough milk. I continue to get better because of this even after giving birth. It's horrible! Is it really supposed to be like this?
Answer: Eat as much as you want! There is no need to “stuff” food into yourself when you are not hungry! The amount of milk produced is primarily affected by how often the baby nurses. WHO observations confirm that only severe malnutrition or dehydration leads to a noticeable decrease in milk supply in women who feed on demand.
Question: I can't live without coffee. But it will also have a tonic effect on the baby, right? Do you really have to give up coffee for many months?
Answer: Indeed, the tonic effect of coffee (as well as chocolate) has an effect on some children. Not for everyone! If you really want to, drink a small cup of weak coffee in the morning and watch your baby. If there are no changes in behavior, drink to your health! 1-2 cups a day will not harm either you or the baby. If your child is clearly more restless than usual, wait 3-4 weeks and try again.
Question: Is it possible to already monitor your figure during breastfeeding? Go on a diet?
Answer: You can and should watch your figure if your mother has such a desire. At the same time, remember the main important points.
1. A woman’s body spends an average of about 500 calories per day to produce milk, which must be taken into account when planning a diet. The nutrition of a nursing mother should be varied and sufficient. In practice, this means that systematic “fasting” for weight loss can provoke a decrease in the amount of milk, and a monotonous diet can lead to a lack of certain elements in the mother’s body, since the body will take the missing components and vitamins for milk from its “reserves.”
2. WHO voices the maximum permissible safe loss of excess weight during lactation - 2 kg per month (500 grams per week).
3. A nursing mother can also support herself through exercise (after consulting a doctor). Moderate exercise does not have a negative effect on lactation. Strength exercises and general overexertion should be avoided.
And finally, a useful sign 
WHO: Impact of maternal intake and health status on micronutrient status
No mammal changes significantly its normal diet while nursing its young. Yes, of course, the cat and monkey do not eat fast food and surrogates, but this is a matter of healthy eating in general, and not restrictions in connection with breastfeeding.
Eat deliciously and feed with joy!
Melnikova Rada, breastfeeding consultant
Sources:
1. “National program for optimizing feeding of children in the first year of life”, Moscow, 2019
2. WHO manual “Feeding and nutrition of infants and young children”
3. Association of Children's Allergists and Immunologists of Russia https://adair.ru/
4. A. Edgar “Anatomy of the breast of a nursing mother” https://www.llli.org/russian/nb/anatomy.html
5. I. Ryukhova “What can a nursing mother eat?” https://www.akev.ru/content/view/4/52/
6. M. Sorokina “Lactase deficiency” https://www.akev.ru/content/view/475/151/ 7. S. Makarov “To eat, or not to eat? That is the question. Or about the role of a nursing mother’s diet in the development of allergic diseases of the baby (for professionals)" https://doctor-makarov.com.ua/blog/27-est-ili-ne-est-vot-v-chem-vopros