Perinatal encephalopathy is a series of diseases of the central nervous system that occur in newborns in the prenatal period, during childbirth or in the early neonatal period. Due to its various manifestations, diagnosing this pathology is very difficult, especially in infancy. Often, the symptoms of encephalopathy are regarded by pediatricians as a manifestation of other diseases. For this reason, due attention is not paid to the treatment of this disease, although it is at an early age that a complete recovery is most likely. As the child grows up, most often, the manifestations of the disease are treated symptomatically, which does not allow the problem to be completely eliminated.
Causes of perinatal encephalopathy
The most common cause of this pathology is birth trauma, but PEP can also be a consequence of hereditary factors, or the result of an unfavorable pregnancy, namely: exposure to occupational hazards, bad habits, or taking certain medications during this period.
Let us dwell in more detail on PEP as a result of birth injuries.
From an osteopathic point of view, the entire complex of central nervous system diseases is a consequence of mechanical disorders. The reasons leading to the manifestation of this disease are: dysfunction of internal organs, circulatory disorders, dysfunction of the spinal column or its individual sections, prolonged fetal hypoxia (oxygen starvation).
Even under the condition of a normal pregnancy, it is at the time of birth that there is a possibility of the child getting injured, since passing between the bones of the pelvis, the fetus makes a complete turn around its axis, which, sometimes, entails structural disorders of the skeleton and muscle tissue. Deviations in the position of the cervical vertebrae are the most common disorder. In the first weeks of a child’s life, the consequences of damage are sometimes completely eliminated by the body on its own. Unfortunately, this does not always happen, and all sorts of deviations in the child’s development can lead to complications in the future.
Perinatal encephalopathy
PERINATAL ENCEPHALOPATHY
Among diseases of the nervous system of newborns, hypoxic vascular damage is in first place. Identification of these disorders, their characteristics, prognosis and an adequate approach to treatment is possible only with a thorough analysis of the neurological status of the newborn.
Perinatal encephalopathies include brain damage that occurs during the period from the 28th week of pregnancy to the 7th day of extrauterine life, when the fetus and newborn have the same physiological reactions with increased vulnerability, primarily of the nervous system. The perinatal period includes:
antenatal period , starting at the 28th week of pregnancy and ending with the beginning of labor, which corresponds to late fetogenesis, during which the fetus is viable outside the mother’s body at any stage of its birth (premature, full-term, post-term);
intranatal period , i.e. the act of childbirth itself (from the onset of labor to the birth of the fetus); early neonatal period (first week of a newborn baby’s life).
There are different classifications of risk factors for perinatal pathology. The most important of them are socio-biological conditions, maternal diseases, complications of pregnancy and childbirth
In the first weeks of life, when the foundations for the child’s further neuropsychic development are laid, careful observation of your baby’s behavior and reactions is especially necessary.
Right now, not later, while the child still does not speak or walk, symptoms such as restless behavior, excessive lethargy, spontaneous shudders, frequent regurgitation during and after meals, bulging eyes, stiffness, inadequate reactions to sound, light, should help you alert. All this may be a manifestation of a neurological disease.
How to distinguish “healthy” crying from “sick” and other symptoms of a neurological disease?
It’s one thing when a baby cries for relatively understandable reasons: hunger, cold, wet diapers. But, you see, any mother should worry if the child cries 20 out of 24 hours a day, and no means can be used to calm him down. It is difficult not to notice the inadequate reactions of a baby (from birth to six months) to the actions of adults: someone enters the room or the doorbell rings - the “neurological” child shudders violently, cries uncontrollably, rolls over, turns blue. Or such a characteristic symptom is throwing back the head. Please do not think that if at 1-2 months a newborn actively arches his back, moves a lot, throws his head back, then he is successful in development. When can you identify an incipient neurological disease, what are its signs and, most importantly, what is the reason for its appearance? The first manifestations of perinatal encephalopathy (as the disease in newborns is often called) can be detected in the maternity hospital. This is a late, weak or painful cry of a newborn; prolonged cyanosis, poor thermoregulation, altered heartbeat, lack of sucking reflex, disturbed sleep, altered motor activity. These conditions may subside within a few days, and the child will subsequently have no abnormalities in the nervous system. In other children, these disorders last longer; they are accompanied by motor disorders in the form of increased or decreased muscle tone, delayed rates of motor and mental development, and problems with the gastrointestinal tract (dysbacteriosis, poor digestibility of food, poor weight gain). Such children require special help - massage, physiotherapy, medications. Only the attending physician can prescribe all this. Therefore, be sure to also find out from the pediatrician everything related to childbirth and the condition of your baby after it: whether he needs consultation or observation from a neurologist. Write down in a separate notebook how the birth proceeded - on time, with forced stimulation, whether the fetus was presented correctly, etc. - all this can be useful not only in the first months of the baby’s life, but also explain a lot even during puberty of your already matured child. If the listed violations pass without a trace, the child can be considered practically healthy, but requires attention. Particular care is required for those children whose neurological disorders not only do not go away with age (by one year in full-term children, by one and a half years in premature children), but their increase occurs. In this case, which can only be determined by the attending physician - a neurologist, we can talk about the transition of perinatal encephalopathy into another disease. Depending on the form and degree, it can be called differently (vegetative-vascular dystonia, neurosis-like syndrome, hydrocephalus, cerebral palsy, etc.) but one way or another it is a chronic disease of the nervous system. In this case, observation and treatment is carried out by many specialists (neurologists, gastroenterologists, immunologists, pediatricians) for many years. The main thing is to have time to properly organize the child’s life not only after birth, but also before, that is, during pregnancy. Much depends on medical workers, whose competence and professionalism often leave much to be desired. But just as much, if not more, depends on the parents themselves. One of the most important risk factors (apart from hereditary factors) is the pathological course of pregnancy. Often, when talking with the mothers of our little patients, it turns out that during the entire nine months of pregnancy the woman slept very poorly, or gained weight unevenly, or often suffered from acute respiratory infections, rhinitis, or bronchitis. So maybe, first, let’s solve our “adult” problems, make pregnancy the best months of our lives, properly prepare (both physically and psychologically) for the birth of a dearly loved baby...
Symptoms of PEP
Symptoms of the disease, depending on the period of the child’s life, have different manifestations. There are three periods in the development of PEP:
- acute (starts from the moment the child is born and continues until the 1st month);
- restorative (up to the first year of life, less often up to 2 years - usually in premature infants);
- outcome of the disease.
During the acute period of development of the disease, symptoms such as tremor of the limbs, increased intracranial pressure with the subsequent development of hypertensive-hydrocephalic syndrome, general lethargy of the newborn, convulsions, shudders, spontaneous motor reflexes, sleep disturbances, muscle tone, and frequent regurgitation are observed.
During the recovery period, these symptoms may be accompanied by movement disorders characterized by complete or partial uncontrolled movements of the child, delayed mental and physical development, and seizures. Signs can appear individually or in combination.
Diagnosis of PEP in neurology. Through the eyes of a specialist
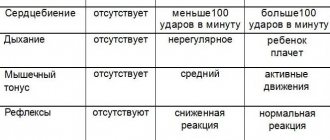
What do neurologists pay attention to during examination? Firstly, on reflexes and muscle tone. Are the reflexes equal on the right and left? Are there any muscle spasms? And vice versa - aren't they contracting too weakly?
Then they check whether the child has signs of increased intracranial pressure. To do this, an ultrasound (neurosonogram) is performed through an open fontanel - they look to see if the ventricles of the brain are dilated. And in conclusion, the child’s behavior is examined, the correspondence of his so-called psychomotor and physical development to his age.
Treatment of PEP with osteopathy
Considering the complexity and course of the disease, the effects of a pediatric osteopath are primarily aimed at damaged areas of the body to eliminate pain and spasms. At the same time, the doctor carries out a number of measures to normalize brain activity. An osteopathic doctor, using special techniques, removes the body deformations remaining after childbirth; they are invisible to the eye, but tangible with his sensitive hands. An osteopath normalizes the functioning of internal organs and the functioning of the nervous system, and removes the tone of skeletal muscles. As practice shows, the likelihood of complete recovery in mild forms of PEP is quite high. Especially when connecting the right osteopathic treatment.
In the presence of a more severe form of the disease, longer treatment will be required, but, unfortunately, this may not provide a complete recovery. Some problems with attention, memory, and coordination of movements can persist in a child not only for a long period of time, but throughout his entire life. Nevertheless, osteopathy leads, if not to complete recovery, then to a significant reduction in the symptoms of perinatal encephalopathy.
The golden rule in the treatment of any pathology is timely treatment. Therefore, the faster violations are identified and eliminated, the greater the likelihood of their complete or at least partial elimination.
Main etiological factors
Depending on the cause of occurrence, there are several forms of encephalopathies in women:
- Dyscirculatory : usually develops in old age against the background of cerebral circulatory disorders.
- Traumatic (or post-traumatic): is a consequence of severe, repeated traumatic brain injury.
- Metabolic : occurs with severe metabolic disorders, endocrine disorders, severe vitamin deficiency, etc.
- Toxic : the main reason is the effect on the brain of ethyl alcohol, industrial poisons, drugs, etc.
- Hepatic : develops with severe liver pathologies, usually at stage III of alcohol dependence or with cirrhosis of another etiology.
- Hashimoto's encephalopathy : extremely rare, occurs due to autoimmune damage to the central nervous system and thyroid gland.
Other types of encephalopathic disorders are described in the medical literature (in particular, HIV-associated, glycine, hypertensive, etc.), but according to experts, these are only subtypes of the listed forms of pathology.
The following diseases and conditions predispose women to the development of encephalopathy:
- pathologies of the endocrine system (acromegaly, thyrotoxicosis, pheochromocytoma, diabetes mellitus, Cushing's syndrome, etc.);
- complicated neuroinfections;
- alcoholism, drug addiction;
- renal, hepatic, cardiac, respiratory failure;
- acute intoxication with heavy metals, carbon dioxide;
- lack of thiamine, cyanocobalamin and other B vitamins, tocopherol, calciferol (in women this can develop during pregnancy, complications during childbirth, etc.);
- atherosclerosis;
- epilepsy;
- chronic hypertension;
- various metabolic disorders accompanied by hypo- or hypernatremia, hypokalemia, pathological changes in the metabolism of calcium and magnesium;
- uncontrollable vomiting of pregnant women, gestosis, etc.
Risk factors for encephalopathy in women include:
- overweight;
- smoking;
- poor nutrition with a predominance of confectionery and flour products, animal fats in the diet;
- sedentary lifestyle;
- chronic stress;
- excessive physical and emotional stress;
- frequent pregnancies;
- chronic depression, severe neuroses, phobic and delusional disorders, etc.