Wet cough due to ARVI in children - what to do?
If a child has characteristic symptoms of ARVI (fever, headache, sore throat, redness of the throat, nasal congestion, runny nose), specific treatment for a productive cough is not carried out. A normally functioning immune system is able to cope with this symptom on its own as it recovers. To help her and speed up the process, you must follow the following rules:
- In the child’s room, optimal temperature (18–20 °C) and humidity (50–60%) should be maintained. It is recommended to regularly ventilate the room, carry out wet cleaning 2-3 times a day, refuse to use heaters and, if necessary, use household humidifiers;
- a prerequisite necessary to cure a child’s severe wet cough is plenty of warm drink (still mineral water, vitamin fruit drinks, herbal teas, milk with honey, etc.). Strict adherence to this recommendation facilitates the removal of sputum, and with it the toxic waste products of the virus;
- If the cause of the cough is mucous nasal secretion flowing down the back wall of the nasopharynx, then for its normal discharge at night and in the morning, experts recommend rinsing the child’s nose with saline solution or irrigating the walls of the nasal cavity with a special nasal spray for children. The condition will be alleviated by raising the pillow higher;
- adherence to strict bed rest during the treatment of ARVI is not necessary (moderate physical activity can significantly facilitate the discharge of sputum);
- Doctor MOM® Phyto ointment can be used as an external remedy for colds in children. This drug contains essential oils of 4 medicinal plants.
At normal body temperature, in addition to the above methods, the child is allowed to do a light percussion massage (gently tapping the back in the lung area with fingertips) to relieve expectoration. To quickly cure a wet cough in a child, one should not forget how beneficial walking outside is ( naturally, if he does not have a high temperature). Fresh air entering the lungs promotes deeper breathing and stimulates the liquefaction and removal of accumulated mucus. An increase in productive cough during a walk is a completely normal phenomenon, due to increased blood supply to the bronchial mucosa and activation of the secretory glands.
Mucolytic therapy in children
E.V. BOYTSOVA
, Doctor of Medical Sciences,
Head. Laboratory of Pediatric Pulmonology, Research Institute of Pulmonology, St. Petersburg State Medical University named after. acad. I.P. Pavlova Inflammatory diseases of the respiratory system in children make up the majority of requests for medical help and represent an important problem in pediatrics and pediatric pulmonology.
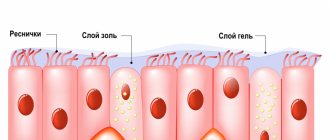
Every year, children suffer from 5 to 12 episodes of viral infection, accompanied by damage to the lower and upper respiratory tract. Normally, air enters the lungs, passing through the upper (oropharynx, larynx) and lower (trachea, bronchi, bronchioles) respiratory tract, during which time the air stream is warmed, moistened and cleaned. Various particles entering the respiratory tract along with air are deposited on the mucous membrane and are then excreted along with bronchial secretions thanks to the bronchial self-cleaning system or mucociliary clearance. Mucociliary clearance is carried out by the movement of cilia of the ciliated epithelium, which ensure the advancement of bronchial secretions, which are secreted by goblet cells and mucous glands. The mucous glands, responsible for the production of mucus in the bronchial tree, appear in the trachea of the fetus at the age of 10 weeks, gradually spread towards the periphery and are located as in adults already in the cananicular stage (17–27 weeks) of antenatal development. At the same time, their structural development ends by the age of 13. At birth, the number of goblet cells is 10% of normal, and by 3 months it increases 4 times. In infants, the secretion of the submucosal glands is less viscous and contains almost no sialic acid. Under normal conditions, the movements of the cilia occur in the more liquid part of the bronchial secretion - in the ash. The sol consists of gland secretions, capillary transudate, interstitial fluid and dissolved chemical compounds. The viscosity of this layer corresponds to the viscosity of the plasma, which ensures effective vibrations of cilia immersed in the sol [1, 2]. The outer gel layer consists of glycoproteins secreted by goblet cells; in addition, it contains lysozyme, albumin, alpha-1-antitrypsin, immunoglobulins A, a complex of lipids, surfactant, interconnected by disulfide, ionic and other bonds. The viscosity and elasticity of bronchial secretions depend on the amount of water and its constituent glycoproteins (mucins). Secretion mucins belong to two different types: 60% hydrophilic acid sialo and sulfomucins and neutral fucomucins - hydrophobic. Under various pathological conditions, this ratio changes; a decrease in the level of sialomucins reduces the water component of the secretion, which is typical for most respiratory diseases. A decrease in the level of the hydrophilic component leads to an increase in hydrophobic fucomucins, which makes the bronchial secretion more viscous and thick. Bronchial secretion of a mucous nature is produced by goblet cells, submucosal glands produce a more liquid serous-mucosal secretion. The largest number of goblet cells is concentrated in the trachea; as we move distally, the number of these cells decreases and they are absent from the bronchioles. In the distal parts of the respiratory tract there are Clara cells, which synthesize phospholipids and surfactant; it is assumed that they can turn into goblet cells during inflammation. The predominant activity of the serous glands leads to the formation of secretion with a low content of glycoproteins. Conversely, hyperplasia of goblet cells with spread to the peripheral parts of the bronchial tree, which is observed in acute and chronic bronchiolitis, bronchial asthma and other diseases of the respiratory tract in children, is characterized by an increase in the content of glycoproteins, the gel fraction and an increase in the viscosity of bronchial secretions [2]. With inflammation in the respiratory tract, the content of microbial breakdown products and exudate (water, proteins, ions) increases significantly, which also increases viscosity. The accumulation of viscous bronchial secretions can lead to ventilation disorders and a decrease in local immunological protection of the respiratory tract, which promotes colonization by pathogenic microflora with a high risk of developing a protracted and chronic inflammatory process [3, 4]. On the other hand, bacterial enzymes and lysosomal proteases can change sialomucins and lead to a loss of the ability to form fibrous structures, which makes the secretion excessively liquid and inelastic, which also reduces the effectiveness of mucociliary cleansing of the respiratory tract [1, 4]. All this makes it relevant to use drugs that affect the secretory activity of the mucosa or secretions through various mechanisms.
When the effectiveness of the cleansing system decreases, a cough appears. Coughing is a normal reaction of the body to irritation, a complex mechanism that helps clear the airways. At the same time, cough is a symptom of a large number of different diseases. There are more than 50 causes of cough; the occurrence of this symptom requires a broad diagnostic search. Most often, cough is associated with pathology of the upper and lower respiratory tract; cough is useful, and the therapeutic goal is to increase its effectiveness. Suppression of cough is required only in cases where it does not serve the function of cleansing the bronchi, for example, with whooping cough, obsessive dry or psychogenic cough [4, 5]. In this case, antitussives of central narcotic and non-narcotic action are used. Narcotic antitussives reduce the sensitivity of the respiratory center, suppress the function of cilia and can cause convulsions. In pediatric practice, non-narcotic drugs of central action are used, which can be prescribed to children from the first months of life.
In case of wet productive cough or bronchial obstruction, centrally acting antitussives are contraindicated. There are a number of drugs with indirect antitussive effects. The administration of bronchodilators helps eliminate bronchospasm and relieve spasmodic cough. Drugs with anti-inflammatory effects, such as fenspiride or inhaled steroids, can also relieve cough by reducing inflammatory changes in the mucous membrane and reducing pathological impulses [5]. The use of antihistamines to treat cough is not advisable because they thicken mucus and impair its drainage.
Currently, there are many drugs that act on sputum and are used for various acute and chronic diseases of the respiratory tract. Traditional expectorants are known to affect the sol layer of sputum. These are reflex drugs, moisturizers and bronchial gland stimulants. Reflex drugs include plant extracts. They irritate the gastric mucosa, stimulate the vomiting center and enhance bronchial peristalsis, reflexively stimulate the secretion of the salivary and mucous glands of the bronchi, which increases the amount of sputum and, as a result, relieves cough. Most of these preparations contain essential oils, which are released through the respiratory tract and increase secretion in small doses, and in higher concentrations cause constriction of blood vessels and a decrease in secretion. Drugs are prescribed with caution at an early age, especially in children with central nervous system damage, since an increase in the gag reflex can cause aspiration and asphyxia. They are not indicated in children with herbal allergies. Resorptive expectorants (bronchial gland stimulants) include salt preparations (potassium, sodium iodides, ammonium chloride). It is believed that the use of these drugs in pediatrics should be limited, since the expectorant effect of iodides is observed in high doses and they have an unpleasant taste [5]. The negative properties of antitussives include the need for their frequent use (every 2–4 hours) [6]. The combination of expectorants and antitussives, according to studies in adults, worsens indicators of external respiratory function [7].
Moisturizing agents, which include drinking plenty of fluids, water and steam inhalations, have a certain effect. Recently, the mucolytic properties of hypertonic NaCL solution have been actively studied. The main mechanism of action of the solution is rehydration of bronchopulmonary secretions, which leads to improved mucociliary clearance. Most studies are devoted to studying the role of hypertonic solution in the treatment of cystic fibrosis. It has been reliably shown that a hypertonic solution is well tolerated (precisely 7%; higher concentrations cause obstruction, lower concentrations are less effective), improves lung function, reduces the number of exacerbations of the bronchopulmonary process, and improves the quality of life of patients [8, 9]. Hypertonic sodium chloride solution is used in the treatment of acute bronchiolitis in young children. Despite the contradictory literature data, the prevailing opinion is that a 3% NaCL solution with beta-2 agonists or adrenaline improves the clinical course of the disease and shortens its duration [7].
The effectiveness of expectorants in acute and chronic respiratory tract damage is significantly inferior to modern mucoactive drugs [6, 7]. Mucoactive drugs change the properties of the gel layer of sputum. Among them, there are drugs with direct mucolytic action, including thiolytics and proteolytic enzymes, and drugs with indirect action - secretolytics and mucoregulators.
Highly active mucolytics are cysteine derivatives with a free thiol group (N-acetylcysteine). Their mechanism of action is based on the rupture of disulfide bonds of sputum proteins, while the polymerization of molecules decreases and the sputum becomes less viscous. It is believed that N-acetylcysteine has a more pronounced ability than other mucolytics to dilute purulent sputum, lyse fibrin and blood clots. N-acetylcysteine is known to reduce goblet cell hyperplasia and mucus hypersecretion [10, 11]. Indications for the use of this drug are clinical conditions in which there is a cough with thick, viscous, difficult to separate sputum (more often this is an exacerbation of chronic infectious-inflammatory, hereditary and congenital lung diseases) [4, 11]. N-acetylcysteine is important in the treatment of patients with cystic fibrosis. The drug is available in various forms: in the form of effervescent tablets, a solution for inhalation and topical use during bronchoscopy and for administration into the sinuses during puncture, for intramuscular administration. When prescribed simultaneously with antibiotics, a 2-hour break between doses should be observed. It has been established that N-acetylcysteine does not affect the bioavailability of amoxicillin and doxycycline and slightly reduces the absorption of cephalexin. The combined use of acetylcysteine with erythromycin significantly increases the absorption of the latter [11]. The use of the drug must be combined with kinesitherapy, since the formation of excessively liquid secretion is possible, which can lead to an even greater deterioration of mucociliary clearance, and this is especially undesirable in young children [1, 2]. The drug has multifaceted chemical properties due to its chemical structure. The antioxidant activity of N-acetylcysteine through direct interaction of the thiol group and free radicals, on the other hand, being a precursor of glutathione, enhances the activity of many enzymes involved in maintaining the balance in the system of oxidants and antioxidants. Associated with antioxidant activity is the ability of N-acetylcysteine to prevent the incidence of acute respiratory viral infections and increase anti-infective immunity, slow down the decline in pulmonary function in COPD in adults, and reduce the rate of progression of pulmonary fibrosis in interstitial diseases [10]. The anti-inflammatory effect of N-acetylcysteine occurs with long-term use in high doses and has been studied in adult patients. It has been established that the drug reduces the adhesion of bacteria to the mucous membrane of the oropharynx, which is a reservoir of endobronchial infection [11]. Perhaps the ability of N-acetylcysteine to reduce the incidence of respiratory diseases in children when administered prophylactically is associated with this mechanism [12]. N-acetylcysteine for intramuscular administration before the age of 1 year is used only for health reasons in a hospital setting due to the risk of “flooding”; other side effects are dyspeptic disorders and allergic reactions.
Dornase alfa is a genetically engineered mucolytic, a drug used primarily for cystic fibrosis in inhalation form, which is a recombinant human DNase. It is known that purulent secretion contains high concentrations of extracellular DNA, which is a viscous polyanion released from collapsing leukocytes that accumulate in sputum as a result of bacterial infection. Dornase alpha causes hydrolysis of extracellular DNA and significantly reduces the viscosity of the secretion. In addition, the drug effectively affects the destructive component of inflammation in the lung tissue, reducing the percentage of neutrophils, lowering the concentration of elastase, interleukin-8 and matrix metalloproteinases in the bronchial contents and promotes the destruction of the biofilm of mucoid Pseudomonas aeruginosa. Studies have demonstrated that dornase alfa is an effective treatment for other chronic lung diseases in children accompanied by bronchorrhea with viscous and purulent sputum [13]. Side effects are generally minor and rare.
Secretolytic mucoactive drugs include derivatives of the alkaloid vasicine (bromhexine and ambroxol). Their mucolytic effect is associated with the depolymerization of mucoprotein and mucopolysaccharide fibers [1, 2]. The clinical effectiveness of ambroxol is significantly higher than that of bromhexine [1, 6]. Ambroxol stimulates the production of surfactant and slows down its breakdown, which improves the sliding of secretions across the epithelium, its fluidity, and increases mucociliary clearance. In case of bacterial infection, with the simultaneous administration of ambroxol and antibiotics, an increase in the concentration of antibacterial agents in the lung tissue was noted. This effect has been described during therapy with amoxicillin, erythromycin, cefuroxime and doxycycline [3, 14]. The anti-inflammatory effect of ambroxol is associated with a suppressive effect on the production of inflammatory mediators by mononuclear cells and an increase in macrophage activity [15]. In case of prolonged exacerbation of asthma in children, it is recommended to combine anti-asthmatic therapy with the use of ambroxol, since in addition to improving the rheological properties of sputum, this drug can suppress the release of histamine, lekotriene and pro-inflammatory cytokines from mast cells [15, 16]. The mucolytic effect of ambroxol is not accompanied by an increase in the amount of secretion. Ambroxol can be used without age restrictions and is available in different forms: syrup, tablets, liquid forms for inhalation and oral administration. There are clinical data indicating an increase in the effectiveness of the drug in children when combining various forms of delivery for chronic bronchopulmonary pathology and exacerbation of bronchial asthma [6]. Side effects are rare and include allergic reactions and dyspeptic disorders.
Modern mucoregulatory agents restore the secretory function of goblet cells and normalize the rheological properties of the secretion. Unlike secretolytic drugs, the site of application of which is pathological secretion, mucoregulators act directly on the glandular cell, regulating its secretory function regardless of the initial pathological condition. This group includes drugs based on carbocysteine. The mechanism of action of carbocysteine is based on normalizing the ratio of acidic sialomucins and neutral fucomucins through activation of sialic transferase and inhibition of enzymes involved in the transfer of carbohydrate residues to the protein base of mucins [2, 3]. Restoring the normal ratio of acidic and neutral mucins in bronchial secretions normalizes the viscosity and elasticity of sputum, increases the efficiency of mucociliary transport and promotes the rapid elimination of inflammation. Under the influence of carbocisteine, the mucous membrane is regenerated, its structure is restored, the number of goblet cells is normalized, which reduces the volume of secretion. Carbocisteine significantly reduces oxidative stress, preventing the formation of free radicals during the inflammatory process [4]. In addition to the direct effect on secreting cells, the effect of carbocysteine on the intracellular transport of ions was discovered, which consists in opening chloride channels and regulating water flow, due to this, additional indications for prescribing the drug for cystic fibrosis appeared. It has been established that in patients receiving therapy with carbocisteine drugs, the concentration of secretory immunoglobulin A increases [17]. Carbocisteine is not effective when used aerosolly; it is highly acidic, which creates the possibility of a negative effect on the gastric mucosa. The combination of carbocisteine with lysine ensures better absorption of the active substance and does not irritate the gastric mucosa. It is believed that this mucoregulator can be used in the early stages of acute respiratory diseases to prevent secretory disorders. In case of chronic lung diseases, good tolerability allows the drug to be taken for a long time; normalization of secretion properties is maintained for 8–13 days after the end of a 4-day course of administration, which allows long-term use of a combination of carbocisteine and lysine in repeated courses with a break [3, 19, 18]. Drugs from the carbocysteine group are characterized by synergism with antibiotics; when used together, there is an increased accumulation of the antibacterial drug in the tissues and secretions of the respiratory tract [4]. The effect of carbocisteine on all damaged parts of the respiratory tract, including the sinuses, as well as the middle and inner ear. The use of carbocisteine has proven effective in the complex treatment of acute and recurrent and chronic otitis in children aged 2 to 12 years [20]. It is known that the main mechanism for the evacuation of mucus from the sinuses and tympanic cavity is mucociliary clearance, since these structures are located away from the general air flow in the nasopharynx and have only a narrow connection with it. The administration of carbocisteine in combination with antibiotics in children and adults with acute and chronic rhinosinusitis demonstrated rapid positive dynamics of clinical symptoms, which is associated with the stimulating effect of the drug on the ciliated epithelium [21]. The effect of carbocisteine has been confirmed in the treatment of chronic adenoiditis; the inclusion of the drug in the treatment protocol led to more rapid improvement compared to traditional therapy [22]. In experiments involving in vitro infection of human tracheal cell cultures with rhinovirus, influenza A virus, and rhinosyncytial virus, the drug inhibited its penetration into the cell, reducing the membrane expression of viral receptors [4]. Other experiments showed the effect of the drug against bacterial pathogens; the use of carbocisteine prevented the adhesion of St. pneumonia to respiratory epithelial cells also by reducing the number of specific receptors [23]. Thus, carbocysteine is the drug of choice for acute and chronic bronchopulmonary pathology, including a combination of damage to the bronchopulmonary system and ENT organs. Recently, the antiviral properties of carbocysteine have been actively studied. The drug can be prescribed from the age of 1 month; it is not recommended for use in children with a tendency to constipation and peptic ulcers.
The choice of a mucoactive agent is determined by the individual characteristics of the patient, the nature and course of the disease, and the characteristics of cough and sputum. In case of acute infection of the upper respiratory tract, occurring with a dry cough, moisturizing procedures, agents with an enveloping peripheral effect, and in older children, centrally acting drugs are indicated. For acute diseases of the upper and lower respiratory tract and lungs at the onset of the disease, accompanied by a dry cough, drugs that stimulate secretion are indicated; for a productive cough, mucoregulators are indicated that normalize mucus formation and the composition of secretions. Viscous purulent sputum, characteristic of patients with chronic diseases of the bronchopulmonary system, requires the use of drugs that destroy mucus polymers. If the distal parts of the bronchial tree are affected, characterized by obstruction and reduced surfactant production in young children, the administration of secretolytic drugs that stimulate the production of surfactant without increasing the amount of sputum will be effective. In case of combined damage to the respiratory tract and ENT organs, mucoregulators are used that penetrate well into the nasal cavity, inner and middle ear.
Literature
1. Mizernitsky Yu.L. Expectorants and mucolytics in the treatment of bronchopulmonary diseases in children. // Tsaregorodtsev A.D., Tabolin V.A. (ed.) Guide to pharmacotherapy in pediatrics and pediatric surgery. M., Medpraktika, 2002. pp. 123-140. 2. Sinopalnikov A.I., Klyachkina I.L. Mucolytic therapy for chronic obstructive bronchitis. // Chuchalin A.G. (ed). Chronic obstructive pulmonary diseases. M.; 1998. pp. 275-291. 3. Ilkovich M.M., Gembitskaya T.E., Panina N.T. Pharmacological correction of mucociliary clearance disorders in patients with acute and chronic lung diseases. Pulmonology. 2009. No. 6. pp. 101-106. 4. Marushko Yu.V. The use of carbocysteine in the treatment of respiratory pathology in children. Modern pediatrics. 2012. No. 4 (44). pp. 1-6. 5. G.A. Samsygina Antitussive drugs in pediatrics. Consilium medicum. Application. 2001. No. 2. pp. 18-22.
You can request a complete list of references from the editor.
What should I give my child for a wet cough?
In some cases, experts recommend taking expectorants as a means of additional treatment for wet children's cough. Among the wide variety of cough remedies, one should highlight Doctor MOM® syrup, made on the basis of plant extracts. It can not only cleanse the bronchi from accumulated pathological mucus, but also have an anti-inflammatory effect. Please note! Taking an expectorant does not negate the need to use other therapeutic factors - regular ventilation, maintaining optimal temperature and humidity in the room, plenty of warm drinks, etc. As for treating a wet cough in a child with folk remedies, it is permissible only after prior consultation with a specialist .
How expectorants and mucolytics work
Expectorants are medications that clear mucus from the airways. Based on their operating principle, they are divided into 2 categories:
- Mucus thinners (secretolytics) – reduce the viscosity of sputum. Some medications increase the concentration of pulmonary surfactants (surfactant), while others destroy bonds in mucus proteins.
- Stimulating expectoration (secretomotor) - stimulate the movement of sputum to the throat. Some drugs provoke a cough, while others increase the production of the liquid component of sputum.
A cough expectorant for children clears the lower respiratory tract of bronchial secretions, which reduces the risk of secondary infections.
Wet cough in a child with bronchitis
If the child’s temperature has already dropped, but there is still apathy, weakness, pale skin and painful coughing attacks (both productive and non-productive), there may be an inflammatory process and the development of complications (bronchitis or pneumonia). In this situation, to confirm or refute the diagnosis, the help of a specialist is required, who will prescribe the necessary studies and give appropriate recommendations for treatment. Attention! Antibiotics should only be taken with the permission and supervision of a physician. Independent choice of antibacterial agents for a child, due to the presence of a large number of contraindications, is strictly prohibited!
Heated discussions continue among pediatricians regarding treatment tactics for the most common and prominent symptom in children with acute respiratory infection (ARI) – cough. And if the theoretical aspects of this phenomenon are well studied, many pathogenetic mechanisms are clear and thoroughly studied, then there are sometimes fundamental disagreements regarding the rational treatment of cough in children against the background of viral respiratory infections [1, 2]. Despite the fact that in Cochrane reviews, from the perspective of evidence-based medicine, we are provided with the results of scientific works that are recommended for use by the doctor, in practice, the choice of a treatment regimen each time causes great difficulties and controversy, especially for the pediatrician. This is quite understandable, because... Each doctor has extensive personal practical experience of successful and controversial clinical cases, his own observations and the opinions of colleagues. The list of medications that exists today is huge, which often leads to polypharmacy and unreasonable prescription of drugs. However, we must make a decision in accordance with approved treatment standards and federal clinical guidelines.
The relevance of the problem remains to this day. Respiratory diseases in children still lead in frequency, reaching 50–73% in the structure of childhood morbidity. Thus, according to the chief freelance pulmonologist of Moscow, Professor A.B. Malakhov, the overall incidence of respiratory diseases among children in recent years remains at a high level and has no tendency to decrease. There are 50 thousand cases of ARI per 100 thousand children (Table 1) [3–6].
The most common manifestation of a respiratory disease is a cough. This type of complaint is most often addressed to a pediatrician. Should he be “treated” against the background of ARI? How often are antitussive drugs used in pediatrics? Drugs that eliminate the cough reflex include the so-called. narcotic antitussives based on codeine and its derivatives and a group of non-narcotic antitussives. The active ingredients for centrally acting agents are oxeladin citrate, pentoxyverine, dextromethophan, butamirate citrate, glaucine hydrochloride. Active substances of peripheral action include prenoxadiazine hydrochloride. The use of such drugs in children may be unsafe. In case of ARI, which is accompanied by the presence of viscous sputum and a wet cough, it is absolutely unacceptable to suppress the cough center and block the cough as the main protective mechanism for clearing the airways. These drugs can cause undesirable effects in children such as increased drowsiness, respiratory depression, constipation, and many others. etc. Therefore, in this clinical situation they are contraindicated.
In pediatrics, there are quite strict indications for the use of antitussive drugs. This is a cough caused by an identified cause of infection: either whooping cough or measles tracheitis. A pediatrician can use an antitussive drug once if a paroxysmal painful cough significantly disrupts sleep and eating, causes vomiting, and the child’s well-being suffers catastrophically. There are also surgical causes of cough, where immediate suppression is really required, for example in thoracic surgery or in acute pneumothorax. For children with severe forms of pathology of the central nervous system, if there is a high risk of aspiration, it is also possible to periodically prescribe drugs that suppress the cough reflex [7].
The simultaneous prescription of mucolytic and antitussive drugs remains a rather serious and frequent medical error. This is where one of the myths about “swamping the lungs” arises. It is impossible, on the one hand, to liquefy sputum, and on the other hand, to simultaneously block the mechanism of its evacuation [8]. Practice shows that expectorants are often used for coughs due to acute respiratory infections and are not only prescribed by pediatricians, but are also actively purchased at the pharmacy by parents. Expectorants, or so-called. secretomotor, drugs should enhance coughing. They differ not only in their mechanism of action, but also in the composition of the active substance. Preparations of plant origin (marshmallow, istoda, thermopsis and other medicinal herbs), terpinhydrate and lycorine, as well as essential oils have a weak thinning effect and stimulate the formation of mucus in the bronchi.
Unfortunately, they also affect the salivary glands, which is an undesirable effect. Preparations based on various salts, such as sodium iodide, potassium iodide and ammonium chloride, can stimulate bronchial secretion and slightly dilute sputum. However, the pediatrician must take into account that this group of drugs has side effects that are significant for the child, for example, the ability to increase the gag reflex, cause various allergic reactions, moreover, these drugs significantly increase the volume of sputum. Many herbal products have a multicomponent composition, and it is impossible to predict how all these components will interact [9]. In addition, the period of action of these drugs is quite short (usually 2–3 hours), there is a need for repeated administration, which in general can lead to an overdose and certain complications [10].
The effectiveness of over-the-counter medications for ARI in children and adults was shown in a 2014 Cochrane review. 29 studies were analyzed: 19 (3799 patients) in adults and 10 (1036 patients) in children [11]. It has been shown that no evidence-based studies have been conducted for expectorants. Antitussives that suppress cough have not been shown to be superior to placebo. And only the group of mucolytic drugs was proven effective compared to placebo.
A 2013 Cochrane Collaboration review of mucolytics (acetylcysteine and carbocysteine) for ARI in children under 13 years of age demonstrated their safety based on 34 (2064 patients) studies using clinical, biological, radiographic and respiratory function parameters . Efficacy was assessed in 6 placebo-controlled studies (497 patients). It has been clearly established that the drugs are effective and have a high safety profile for children over two years of age. It should be noted that in clinical studies there were not a single case of the so-called. swamping of the lungs syndrome and not a single case of bronchospasm, which is sometimes feared by practicing pediatricians [12].
Modern mucolytics are created on the basis of various chemical formulas, which explains their different mechanisms of action (Table 2). Looking at the information in the table, you can decide which mucolytic is advisable to use in a specific clinical situation and choose not by name, but by the mechanism of action of the active substance.
Acetylcysteine and ambroxol are included in the list of vital and important medications, and dornase alfa according to the “7 nosologies” program is included in the basic therapy of cystic fibrosis. In order to assess the effectiveness, tolerability and safety of mucolytics for children with ARI, a study was conducted on 259 children with acute and chronic bronchopulmonary pathology under the age of 15 years. Children received treatment for 5–15 days: 92 children received acetylcysteine, 117 - ambroxol, 30 - bromhexine and 20 - mucaltin. The authors showed that the best clinical effect in children with acute bronchitis was obtained with the use of acetylcysteine. When prescribing bromhexine and ambroxol, a pronounced mucolytic effect was also noted, but at a later date from the start of treatment.
In the attacking period of bronchial asthma, when acetylcysteine was prescribed in complex therapy, the best effect was achieved by children of the younger age group [7, 13]. In addition to the mucolytic effect, the acetylcysteine molecule has two additional effects. Thanks to its triple effect - mucolytic, antioxidant and anti-inflammatory - the use of acetylcysteine in ARI helps reduce the duration of cough, reduce the intensity of the inflammatory reaction and shorten the duration of the disease. The mucolytic effect of acetylcysteine is due to the presence of an SH group in the acetylcysteine molecule, which breaks the disulfide bonds of acidic mucopolysaccharides of sputum, directly changes the rheological properties of sputum, reduces its viscosity and adhesiveness. The direct antioxidant effect of the acetylcysteine molecule is explained by the fact that reactive SH groups bind to free radicals and thus neutralize them. And the indirect antioxidant effect occurs due to the ability of acetylcysteine to influence the synthesis of glutathione. The anti-inflammatory effect is associated with the ability of this molecule to increase cell protection from the damaging effects of free radical oxidation inherent in the inflammatory response. The practical significance of this triple action for patients is shown in a research work in which 60 children aged 2 to 10 years were observed with clinical manifestations of acute respiratory disease and with difficult to separate sputum (acute bronchitis, including with obstructive syndrome, acute stenosing laryngotracheitis, pneumonia).
As a result of observation, it was shown that the use of acetylcysteine in the complex treatment of acute respiratory diseases in children contributes not only to a more rapid achievement of a productive cough with improved bronchial drainage function and a reduction in the duration of cough, but also to a more rapid relief of symptoms of intoxication and fever, which contributed to a reduction in hospitalization time children with acute respiratory diseases [14].
The safety and good tolerability of the drug can be judged by how it is tolerated in chronic conditions, for example, chronic bronchitis, when therapy is carried out in long courses. A 2015 Cochrane review found that studies involving 9367 patients showed a reduction in exacerbations when mucolytics were used for more than 10 months. All mucolytics used (including acetylcysteine, carbocysteine, ambroxol and bromhexine) turned out to be safe, and all were well tolerated [15]. However, this review included studies from adults. In children, long-term use of mucolytics for 12 months was shown in 4 studies involving 149 children over two years of age with cystic fibrosis. The results obtained did not reveal significant clinical differences between acetylcysteine and ambroxol; there were no serious side effects with both inhalation and oral administration; the drugs were well tolerated [16, 17].
An important practical question for a pediatrician: how do mucolytics work for upper respiratory tract infections? In the indications for the use of acetylcysteine and carbocysteine, unlike other mucolytics, their use is also prescribed for upper respiratory tract infections, such as catarrhal and purulent otitis media, acute and chronic sinusitis. This is understandable, since the mucous membrane of the respiratory tract begins with the nasal cavity and ends deep in the bronchioles. Therefore, the laws of inflammation during infection, the pathogenesis of the development of acute bronchitis and acute rhinitis are similar throughout the respiratory tract. The acetylcysteine molecule will exhibit its mucolytic and anti-inflammatory properties equally in the lower respiratory tract and in the upper. Otorhinolaryngologists widely use acetylcysteine in their practice [18–20].
During an acute infection, inflammation occurs on the mucous membrane of the respiratory tract and a viscous secretion is formed, which leads to blocking of mucociliary transport, mucostasis develops and, as a result, microbial colonization. ARIs are usually caused by viruses, but bacterial complications may require antibiotic therapy. The review showed that all mucolytics, if necessary, combine well with antibiotics (Table 3) [21, 22].
In some studies, it was shown in relation to the acetylcysteine molecule that it increases the clinical effectiveness of antibacterial therapy by suppressing the growth and destruction of bacterial biofilms [23, 24]. A comparative study was carried out on the effectiveness of mucoactive drugs in reducing the viability of biofilms produced by S. aureus strains [25]. It was found that the activity of acetylcysteine was 5.5 times higher than that of ambroxol and bromhexine.
The combination of acetylcysteine with penicillin antibiotics for acute bronchitis and pneumonia helps to reduce the intensity of cough already by the third day from the start of treatment, and with cephalosporins (for example, cefuroxime) increases effectiveness for bacterial infections of the respiratory tract [26–29].
Each time, the pediatrician must choose not only the drug itself, but also the most effective route of administration. Today, acetylcysteine and ambroxol have dosage forms in the form of solutions for nebulizer therapy, unlike carbocysteine. This is definitely an innovative technology. But the nebulizer method of administration also has its drawbacks. First of all, the presence in the family of a sick child of the device itself - modern and of good quality. The psychological characteristics of the child do not always allow the inhalation procedure to be carried out. It takes a lot of time and requires complete physical and emotional commitment. There is no systemic effect with this route of drug administration. This can be considered a positive fact [30]. But, in the case when it is necessary to influence not only the lower respiratory tract, but also the upper, to relieve the symptoms of intoxication, you will need to take a mucolytic orally. Nebulizer therapy is deservedly widely used both in hospitals and in outpatient practice. But in most cases there is no need for inhalation delivery, because The bioavailability of drugs when taken orally is sufficient. It is necessary to rationally balance decision-making depending on the specific clinical situation of the patient.
In normal practice, it is not advisable to prescribe multiple mucolytics at the same time. There is no need to enhance the mucolytic effect with drugs from one drug group. Moreover, this can be considered a medical error, because in a child with ARI, excessive sputum production can be caused, which the baby will not be able to effectively evacuate, and complications may arise in the form of “swamping of the lungs syndrome,” obstruction with respiratory failure, and even pneumonia. When treating patients with chronic bronchitis, for example, against the background of cystic fibrosis or severe congenital malformations of the bronchi with severe mucostasis, this practice, on the contrary, is successfully used. Using different properties of active molecules, it is possible to create the most effective combinations of mucolytics, as well as use different routes of their administration (for example, alternating inhalation with oral administration) [31].
It should be noted that acetylcysteine is recommended by the Standards of Primary Health Care for ARI and Sinusitis; acetylcysteine and ambroxol are included in the standards of outpatient care for acute bronchitis. These regulatory documents enable the practitioner to use these medications reasonably [32].
Thus, the main practical conclusions and recommendations for selecting therapy for ARI for children include the following:
- for uncomplicated ARI in children, acetylcysteine and ambroxol, which have the same proven effectiveness and have a high level of safety, can be equally used for mucolytic purposes. It should be borne in mind that acetylcysteine will act somewhat faster, because is a direct mucolytic, but not “stronger”;
- in case of acute infection, which occurs with symptoms of bronchitis and rhinosinusitis, it is advisable to use acetylcysteine, which will dilute not only bronchial, but also nasal secretions, and also reduce inflammation in the paranasal sinuses. For children over two years of age, ACC® (acetylcysteine 20 mg/ml) can be recommended in a child-friendly form - syrup without sugar, alcohol and dyes;
- if ARI occurs in addition to cough with severe symptoms of intoxication (high fever, severe weakness), you should choose acetylcysteine, not only due to its mucolytic, but also antioxidant and anti-inflammatory properties, which will neutralize these symptoms;
- in case of prolonged or chronic inflammation in the respiratory tract, it is advisable to use ambroxol, using its property to stimulate the synthesis of surfactant, which decreases with prolonged bronchitis;
- if there are indications for prescribing antibiotics, a combination with acetylcysteine is preferable, which has the property of destroying bacterial biofilms and thus can enhance the effect of the antibiotic;
- for children under two years of age, ambroxol remains the drug of choice (any dosage forms, including solutions for inhalation, but you must remember about drainage);
- it is possible to combine the ways of administering mucolytics depending on the situation: ½ of the daily dose should be prescribed in the form of nebulizer inhalation, and ½ as a daily dose orally.