Causes of suffocation in children
Asphyxia is suffocation caused by compression of the respiratory tract, closing of their lumen with mucus, food, compression of the neck, chest and abdomen and leading to oxygen starvation and excessive accumulation of carbon dioxide in the tissues and cells of the body, which threatens severe disorders of the nervous system, breathing and circulation .
In a newborn, this condition can be caused mainly by two reasons:
- The presence of an external obstacle to free breathing : a diaper hung on the crib railing or a corner of a blanket may fall on the child’s face; The baby may burrow or “crawl” under the blanket when he sleeps restlessly or when he wakes up. It must be said that newborns have an unconditioned crawling reflex: the child lies on his stomach and if something hard gets under his feet (the side of a crib, changing table), then the baby is able to push off the object with his legs and make crawling movements, lifting and moving his buttocks forward . In this case, the head, shoulders and arms passively move along the surface. Getting tangled in the strings of a duvet cover, bumper, or rattles placed low on the crib can also cause suffocation. Long laces from bonnets, pacifiers, and jewelry chains can wrap around a child’s neck, causing suffocation, which is complicated by the baby’s efforts to free himself from them. Sleeping together in the same bed between the baby and parents, and even more so - sleeping together in the same bed with older brothers and sisters is also dangerous due to possible suffocation of the newborn. They may accidentally cover his head and press the baby's face to his body. It is also dangerous to put your baby to sleep on a bed with a hydromattress. The baby may find itself between its fixed parts and the movable mattress. You should not trust older children too much to care for your newborn. They may be too zealous in caring for the younger one: wrapping him up too much, covering him with a blanket, or feeding the child food that is inappropriate for his age, for example, sharing cookies with him, especially if the baby is crying.
- The entry of foreign bodies into the respiratory tract (most often these are food masses during regurgitation or vomiting) is the cause of accidents. This is especially dangerous for premature, weakened children, in whom all protective reflexes are not yet sufficiently developed. In such babies, breathing may stop during sleep, without the appearance of a characteristic cough as a defensive reaction when the body tries to free itself from a foreign body.
Predisposing factors
If breast milk enters the larynx, a severe cough occurs with short-term interruption of breathing. A newborn who has choked may experience changes in the color of the skin (they become bluish) and more severe abnormalities. The main cause of conditions in which breast milk is refluxed into the respiratory tract is a violation of the rules of feeding a newborn. They can be represented by the following factors:
- Associated with the rapid flow of milk or other fluid. It is caused either by the small size of the nipple, which is not able to let milk through in doses, or by a large hole on the latex nipple (if the infant is bottle-fed),
- Associated with breast fullness. A baby can easily choke if there are long intervals between feedings,
- Active sucking movements of the newborn, leading to excess milk in the oral cavity,
- The horizontal position during feeding poses a serious risk of choking.
Important to remember! In classic cases, liquid entering the respiratory tract of newborns does not pose a life-threatening risk. Panic, fuss and unnecessary actions are what you should not do. They can aggravate the situation. Only clear, consistent assistance will help avoid serious consequences!
External signs of asphyxia
The baby exhibits motor restlessness, choking, the child gasps for air, and there may be a muffled, muffled cry (but it happens that children do not cry and thus do not attract attention to themselves). Previously uncharacteristic wheezing, whistling sounds may appear - so-called stridor breathing, hoarse voice or its complete absence, unexpected, paroxysmal cough, shortness of breath, retraction of the supraclavicular fossa, intercostal spaces, abdomen, frightened eyes, formation of a large amount of saliva, rapid and then slow heartbeat, decreased breathing. Characteristics of suffocation are cyanosis (bluish discoloration) of the face, limbs, body, loss of consciousness, convulsions, complete muscle relaxation, and lack of reflexes.
What to do if a child chokes?
In such a critical situation, there is no time to wait for medical help, and you must rely primarily on yourself.
- Ask people nearby to call an ambulance, and do not waste your precious time on this. Clear the child's airways: remove the diaper, blanket from the face, remove objects that are squeezing the neck, wipe food from the face that the child has regurgitated. Try using a rubber enema bulb to suck out the contents (food masses) from your mouth and nose. The oral cavity can be freed from possible foreign objects with a finger wrapped in a napkin or handkerchief. If a child cries, wheezes, or coughs, it means that the airway is partially passable. The baby needs to be helped to clear his throat, turn the baby upside down, pat between the shoulder blades or press the root of the tongue with a spoon to induce a gag reflex. You can even take the child by the legs, turn him upside down and slap him on the back a few more times. You can also simulate a cough by sharply squeezing the sides of the lower chest with your hands and try to push the object out. In most cases, these measures are sufficient to push out the foreign body.
But do not try to grab an object stuck in your throat with your fingers - this can push it even further and cause a reflexive stop in breathing.
- If these measures are not successful, the child does not cry, does not breathe, the skin color remains bluish, the pulse and heartbeat are not detected, it is necessary to begin resuscitation measures: artificial respiration and chest compressions, which are performed simultaneously. Note the time when you started them.
How can you tell if a child is choking?
To begin with, every parent needs to remember that if a child is able to cry and call for help, it means that his airways are not blocked and the body will cope with the problem on its own. There is no need to vigorously hit your baby on the back or shake his legs. The cough that appears in such cases is the best helper, and you simply control the situation and calm the baby.
It is necessary to show concern and provide urgent assistance to a child if the following signs appear:
- the child’s eyes are wide open, and there is complete panic in them;
- the child is not able to inhale air normally and cry, his voice becomes hoarse or disappears altogether;
- the baby opens his mouth wide, salivation increases;
- the skin first turns red and then begins to turn blue;
- older children wrap their hands around their throats;
- in particularly critical situations, the baby may lose consciousness.
All of the above indicates that a foreign object has blocked the child’s airways and is preventing the normal flow of air. In this case, we immediately call an ambulance (tel: 03, 112, 030), and we ourselves begin to provide first aid.
We help children under one year old
(watch the video at the end of the article)
Most often, babies under one year old choke while feeding: milk, large pieces of food, water. The most common reason for this is incorrect posture. How to help the baby?
- One way is to raise the child's arms up. Few people have heard of this method, and at first glance it seems too simple and ineffective. However, this position helps to expand the airways and improve the breathing process.
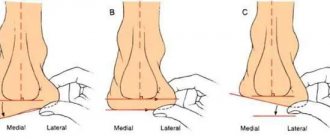
- If this does not help, you need to place the child on his tummy on your hand and with the edge of your palm make 5 pats between the child's shoulder blades.
- If a child chokes on a small object or pieces of food, you need to lift the baby by both legs (Fig. 3) or by pressing on the root of the tongue to induce vomiting, this is often enough and no additional manipulation is required.
If a child breathes normally, but coughs a lot, it means that pieces of food are stuck not in the respiratory tract, but in the larynx. Usually, due to coughing or vomiting, the foreign body comes out on its own.
The situation is much more serious when food or a foreign object gets stuck in the child’s respiratory tract. In this case, untimely or incorrectly provided assistance can lead to suffocation and even death. The main signs of such a jam are that the baby cannot scream and cry, waves his arms and sucks in his stomach. There are several ways to clear a child’s airways:
- If a child chokes on water or milk, he begins to cough heavily (chokes on a cough, breathes noisily), you need to turn his back to you, hug him with one hand, while simultaneously pressing on the stomach area, tilt the baby forward and pat him on the back.
- If a child chokes on milk, water or saliva, but the previous method did not help, you need to place him on his back so that his head is lower than his body. We place the middle and index fingers under the baby's chest bone. We make five pressures, making sure that after each of them the baby’s sternum straightens. You need to alternate between pressing and patting on the back from step 1. before the ambulance arrives (see Figure 2).
- If a hard foreign object gets stuck (an icicle candy or the eye of a favorite toy), we place the child face down on his arm. The head should be below the chest. With our free hand we clap the child between the shoulder blades (Fig. 2). The second option is to take the child by the legs and lower him upside down. We clap between the shoulder blades in the same way (Fig. 3).
(Figure 2) Place the baby face down in your arm so that the head is lower than the body.
Using the heel of your free hand, clap 5 times in a row between the child's shoulder blades. After each pop, check to see if the airway blockage has cleared. If the foreign body cannot be removed, turn the child onto his back. Place two fingers on the baby's sternum and make 5 presses, pressing the sternum to a depth of 1-2 cm and allowing the sternum to straighten after each press, without removing your fingers from it. If these measures do not help, call the ambulance again and make sure that the call was accepted. Until the ambulance arrives, continue to provide first aid, alternating between patting the back and squeezing the chest. If at any point the child loses consciousness, begin artificial respiration and chest compressions. (Figure 3) we take the child by the legs and lower him upside down, clapping between the shoulder blades. All pressing and patting performed should be gentle but sharp. When performing such movements with significant force in babies under one year of age, there is a risk of rupture of internal organs.
Some sources give fundamentally incorrect advice - examine the child’s larynx with your finger and try to remove the foreign body. Perhaps this method will help if something soft, such as cotton wool, is stuck. But in most cases, you run the risk of simply pushing the stuck object even deeper, and then you definitely cannot do without surgical intervention.
[sc:ads]
First aid for a child over one year old
(watch the video at the end of the article)
The most important thing here is the absence of panic. Children older than one year already understand more, and therefore excessive concern and nervousness will only aggravate the child’s mental state at this already difficult moment.
The basic principles of providing assistance here are the same as for children under one year old. If pieces of food or foreign objects get stuck in the larynx, you need to induce vomiting or lift the baby by both legs. Although sometimes the child is able to clear his throat on his own.
If the manipulations listed in the previous section do not help, place the baby face up on a flat surface and turn his head slightly to the side. Now you need to perform several presses on the upper abdomen and lower part of the sternum in an upward direction. This method helps to push the stuck object out of the respiratory tract.
Another way: Give 5 slaps on the back
Sit or stand behind your baby and place your hand diagonally across your chest. Tilt your baby forward a little so that he is leaning on your hand. With the palm of your free hand, give five firm and separate slaps on the child's back, directly between the shoulder blades.
When a candy, piece of food or any other foreign object gets stuck, the Helmich method is effective for children over one year old. It consists of the following:
- we stand behind the child (if he is small, we kneel);
- We wrap our arms around the baby’s waist;
- clench one hand into a fist and place it between the ribs and the baby’s navel with the thumb inward;
- We clasp the fist with the second palm;
- We spread our elbows to the sides and press on the child’s stomach in the direction from bottom to top.
Such movements must be performed until a piece of food jumps out of the child’s respiratory tract. Remember that the method cannot be used on children under one year old.
Bend the child forward and use the heel of your hand to make five strong claps in a row between the shoulder blades. Between pops, check to see if the blockage has cleared. If the airway cannot be cleared, proceed to the next step. Place one hand on your back and the other in the center of your chest. With the hand that lies on the chest, make 5 strong pressures, much like a heart massage, but slower and sharper. If these measures do not help, call an ambulance, and until it arrives, alternate 5 claps on the back and 5 chest compressions.
What to do if the child stops breathing?
The child may stop breathing due to a spasm in the throat, which in most cases occurs due to the baby’s stressful state.
You can restore breathing as follows:
- place the child on the floor on his side;
- tilt his head back a little;
- lift your chin.
If such manipulations do not help, you should immediately begin performing artificial respiration. It is done as follows:
- Place the baby on his back on a flat surface;
- we tilt the baby’s head back and open his mouth;
- check that there are no foreign bodies in the child’s mouth;
- take a deep breath;
- cover the child’s nose and mouth with our mouth and exhale the collected air;
- repeat 2 times. If the child's chest rises with a sigh, then you are performing artificial respiration correctly. If your baby's chest does not rise, this means his windpipe is still blocked and you should return to first aid procedures to remove the foreign body;
- Next, we place the palm of one hand on the child’s chest between the nipples, cover it with the other hand and make sharp pressing movements. Each press should be strong and fast and should press down the baby's chest about 5 centimeters. Allow your chest to return to its starting position between each compression;
- alternate 15 pressures with air inhalation.
Video - First aid: how to perform artificial respiration on an adult and an infant
Even if everything went well, you should not ignore the help of the ambulance that arrived in time. It is possible that the airway has been injured by a foreign object and you will need the help of a specialist.
Is the child not breathing? Let's start resuscitation!
First of all, you need to put the child on his back on a flat, hard surface (table, floor, ground), and put a diaper or clothes rolled up in the form of a cushion under his shoulder blades. Then the victim’s head will be thrown back and the tongue will not sink, preventing the passage of air into the respiratory tract. After this, the child must be undressed, removing all constrictive clothing.
Resuscitation begins with artificial respiration . In newborns, it is carried out both in the nose and in the mouth at once. Having previously taken a shallow breath, tightly cover the child’s mouth or nose with your mouth and exhale briefly with approximately the volume of air that can fit in your mouth, but no more, since inhaling the entire “adult” volume of the lungs can lead to rupture of the child’s lungs. There is a criterion for the effectiveness of artificial respiration - excursion (movement) of the victim’s chest, similar to breathing. But make sure that when inhaling air, the child’s cheeks do not swell: this indicates that air is not getting into the lungs and the help is ineffective. Check whether your lips are tightly wrapped around the victim’s nose or mouth, whether the head is thrown back sufficiently and whether the tongue is blocking the airways, and whether all foreign bodies have been removed from the oral cavity. Press your lips more tightly to the child’s face, tilt your head back again, or additionally free the oral cavity from foreign bodies. In children under one year of age, the frequency of insufflations is approximately 20 per 1 minute.
| Note. The easiest way to detect pulsation in a newborn is on the large fontanelle, as well as on the brachial artery: take the child’s hand away from the body and turn it palm up. In the middle third of the shoulder on the inside, use your index and middle fingers to feel the pulse between the two muscles. It is difficult to check the pulse in the carotid artery and neck in newborns due to the fact that the neck is still short and the skin on it has numerous folds. In order to check the heartbeat, you need to place your palm on the baby's chest, on the area of the left breast. If you can feel the heartbeat, but there is no pulse in the arteries, then cardiac activity is considered insufficient and resuscitation measures are necessary. Such measures are also necessary in the absence of a heartbeat. |
After each inhalation it is necessary to perform an indirect cardiac massage .
You need to find a point on the baby’s chest to press on. The guideline is this - it is located one finger width below the line mentally drawn between the nipples, along the left edge of the sternum (approximately in its lower third).
Children under one year old need to sharply press on this point with two fingers - the index and middle, while the hands should be kept strictly perpendicular to the victim’s body, not bent at the elbows, efforts should be made only with the hands, and not with the whole body, that is, you cannot transfer your body weight to hands so as not to damage the child's ribs.
The child's chest should be clasped with both hands (thumbs resting on the indicated area) and squeezed vigorously. The frequency of chest compressions in newborns is 120 times per minute. Remember that when performing artificial respiration, cardiac massage is interrupted so that it does not interfere with the respiratory movements of the chest.
The criterion for the effectiveness of chest compressions is the appearance of a pulse in the fontanelle and large vessels (see above). Therefore, when performing resuscitation, check for pulsation approximately once a minute. If the pulsation is restored, the indirect massage should be stopped, and artificial respiration should be continued until spontaneous breathing is restored. If there is no pulse, continue resuscitation and monitor the pulse every minute. Sometimes it is difficult to determine the pulse due to low filling of the vessels or as a result of an error in finding the point of palpation for the pulse. Therefore, after 3-5 minutes, it is recommended to interrupt the indirect cardiac massage and artificial respiration and determine the presence of independent heartbeat, spontaneous breathing, and pupil size by external signs. Narrow pupils are a sign of recovery of brain function.
What should you achieve as a result of all resuscitation efforts? Restoring the vital functions of the body, i.e. the occurrence of spontaneous breathing, pulsation, heartbeat, constriction of the pupils and their reaction to light, changes in skin color from pale, bluish to pink.
The child should then be taken to the hospital for a comprehensive examination, especially if respiratory arrest occurs due to regurgitation or vomiting. Food masses that enter the bronchi from the stomach are acidic due to gastric juice and thus act as an aggressive environment for the delicate mucous membrane of the respiratory tract, leading to its damage and inflammation. Most likely, in this case, a sanitary bronchoscopy will be performed (insertion of an optical device into the bronchi, which allows you to examine the bronchi and, if necessary, wash them), an x-ray, and antibiotics will be prescribed.
If, during the provision of resuscitation assistance, the heartbeat and breathing are not restored, and the pupils remain wide, then indirect cardiac massage and artificial respiration should be continued until the ambulance arrives or until cardiac and respiratory activity. The decision to stop resuscitation is made by the doctor.
To increase the lifespan of the cerebral cortex in case of disruption of vital functions, in the very first moments after loss of consciousness, cover the child’s head with something cold (a heating pad, bottles of cold water, ice from the refrigerator, a bag of frozen vegetables, frozen meat, etc.) .
If at any stage of resuscitation the child begins to vomit, turn him on his side, use your finger to clear the vomit from his mouth, put him back on his back and continue resuscitation.
What to do and how to help your child
If a situation arises in which a baby chokes on milk, you need to do the following:
- Stop feeding immediately
- Place the newborn in an upright position
- Take a newborn who is choking in your arms so that his back is facing the person providing assistance, tilting his head slightly forward and downward. In some cases, the baby is placed with his stomach on the forearm of the left arm and hand,
- Place your index finger in the oral cavity, opening the entrance to it slightly by moving the lower jaw downwards,
- Tap with a straightened palm on the back in the interscapular area.
- The baby should remain in this position until the coughing attack is stopped and normal breathing is restored,
- Against the background of ongoing activities, it is imperative to monitor the condition of the newborn who has choked, his consciousness and breathing. If they are absent, an ambulance is called urgently and resuscitation measures begin. First of all, the patient is placed in a supine position with the head extended, and the patency of the airways and oral cavity is controlled. Artificial respiration is performed in combination with chest compressions. (Press with two fingers just below the inter-nipple line with a frequency of 100-120 presses per minute, the chest should “move” 1-2 cm, the ratio of the number of breaths to the number of presses: 1:5)
Newborn children have imperfect mechanisms for regulating the body's vital functions. Sometimes it happens that even unconditioned adaptive reflexes do not have time to adapt to changing environmental conditions. One of the most common conditions, such as the consequences of impaired swallowing reflex and what to do if a newborn chokes, is discussed in this article.
Prevention of suffocation in a newborn
- After each feeding, the baby should be given the opportunity to burp the air swallowed with food. To do this, you need to hold it vertically for some time and under no circumstances put it down immediately after feeding. Some babies (especially premature or weak ones) may burp repeatedly while in the crib. To prevent inhalation of contents, always turn the infant's head to the side. If regurgitation is frequent and profuse, then this is a reason to consult a doctor.
- When choosing children's bedding and clothing, preference should be given to products without all kinds of ties, ribbons, etc. Instead of a baby blanket, you can use a special sleeping envelope; do not use too large “adult” blankets. You can use special mesh blankets for babies.
- You should not leave older children alone near the newborn for a long time, hoping for their maturity and prudence, and also put the baby to sleep in the same bed with them. And sleeping together in the same bed with parents is not safe from the point of view of possible asphyxia.
- Co-sleeping can also be a risk factor for baby suffocation. Although many new mothers bring their babies to bed with them, it is still optimal to sleep in the parents' bedroom, but not in the parents' crib. Place the baby crib next to yours and lower the side rail. On the one hand, this will ensure the safety of the baby, on the other hand, you will be in close proximity to your child and you will not have to jump up several times at night. It will be convenient for you to feed the baby at night, and then, without getting up, transfer him to the crib.
- To prevent respiratory arrest, it is preferable to place the child alternately on one side or the other, since there are some disadvantages in the positions on the back and on the stomach.
Advertising
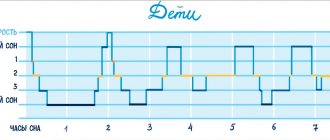
Scientists have identified a certain relationship between a child sleeping on his stomach and an increase in the incidence of sudden infant death syndrome (SIDS). This is the name for the sudden death of a child in the first year of life (especially the first to fourth month) for unknown reasons, against the background of complete health, often at night and in the early morning hours. Neither a detailed study of the baby’s medical history nor the results of a pathological examination help explain the reasons for this phenomenon. So far, only the factors influencing sudden death have been clarified, by which it is possible to identify children at risk and carry out preventive measures for them. However, in the prone position, gases are released more easily from the baby’s swollen belly, the back muscles are strengthened, and the correct position of the hip joints is formed. And if you don’t risk putting your baby to sleep on his stomach at night, then you can easily do this during the day when the baby is under your control. But the supine position also has its disadvantages. In this position, children suffering from regurgitation and vomiting may choke on vomit. And with an underdeveloped frenulum, the tongue can also easily sink.
In conclusion, we note that you should always think about the safety of the baby. He is very defenseless and can only help himself by calling on those around him to cry.