What is polio
Poliomyelitis is an acute infectious viral disease that affects the nervous system.
For this reason, irreversible flaccid paresis and paralysis can form. This happens when the virus infects the motor neurons of the spinal cord. In rare cases, the neurons responsible for the functioning of the respiratory muscles are affected. The disease mainly occurs in children. Today, most countries of the world (including Russia) are considered free from poliovirus. The last polio epidemic in Europe and the United States was recorded in 1988. Thanks to mass vaccination, it was possible to radically reduce the incidence (by more than 99%). Isolated cases of the disease are recorded in Afghanistan, Nigeria, Syria, Angola, India, Pakistan and some other countries.
Polio in numbers: WHO data
The World Health Organization provides the following facts about polio¹:
Most often, poliovirus affects children under 5 years of age.
Every 200th case of infection leads to irreversible paralysis. In 5-10% of paralyzed people, paralysis of the respiratory muscles develops, which leads to death.
Over the past 30 years, the number of cases of infection with the wild strain has decreased by 99%, from 350 thousand to several dozen cases.
The risk of spreading poliovirus remains until it is completely eradicated. If the polio virus is not combated, then in 10 years the number of cases may again reach 200 thousand or more.
Polio vaccination has prevented over 16 million paralysis.
Frequently asked questions about polio
frequently asked questions about polio
December 11, 2015
1. What is polio?
Poliomyelitis is a highly contagious disease caused by the poliovirus. It attacks the nervous system and can cause paralysis or even death in just a few hours.
2. How is polio transmitted?
Wild poliovirus (WPV) enters the body through the mouth through water or food that has been contaminated with feces from an infected person. The virus multiplies in the intestines and is shed in the feces of an infected person, through which it can be transmitted to other people.
3. What are the symptoms of polio?
The initial symptoms of polio are:
- heat
- fatigue
- headache
- vomit
- neck stiffness
- pain in the limbs.
4. Who is at risk of contracting polio?
Polio mainly affects children under 5 years of age.
5. What are the consequences of polio?
Poliomyelitis causes the following consequences:
- One in every 200 people infected with polio will experience permanent paralysis (usually in the legs).
- Of those paralyzed, 5% to 10% die from respiratory muscle paralysis caused by the virus.
6. Is there a cure for polio?
No, there is no cure for polio. Polio can only be prevented through immunization. There is a safe and effective polio vaccine, oral polio vaccine (OPV). OPV provides essential protection for children against polio. If used repeatedly, it protects the child for life.
Global fight against polio
7. What is the Global Polio Initiative?
In 1988, governments created the Global Polio Eradication Initiative (GPEI) to rid humanity of the disease forever. The initiative is a global partnership involving national governments, WHO, Rotary International, the US Centers for Disease Control and UNICEF. Since the creation of the GPEI, the number of polio cases worldwide has decreased by more than 99%. Just 20 years ago, polio caused paralysis in 1,000 children every day. In 2010, 1,349 children were paralyzed.
8. Where is wild poliovirus still circulating today?
Polio transmission has never stopped in 3 countries - Afghanistan, Nigeria and Pakistan. However, polio can and does spread from these countries to neighboring and more distant countries. It must be remembered that the emergence of polio anywhere is a threat to children throughout the world. He has no regard for boundaries or social status and moves easily.
9. Can polio spread to other polio-free countries?
Polio does not respect borders: any unvaccinated child is at risk. For every case of paralysis, between 200 and 1,000 children become infected asymptomatically. Therefore, identifying polio is difficult, as is preventing its movement. Children living in areas where immunity levels are low are especially vulnerable. The best defense against imported polio is eradication of the virus. Only in this case will all children be safe.
10. What needs to be done to eradicate polio?
To stop polio we must:
- engage the entire community in efforts to reach every child left behind;
- develop special plans to reach children from mobile, migrant, conflict zones or remote areas;
- strengthen routine immunization, which is the nation's best defense against polio;
- improve surveillance in high-risk areas;
- encourage governments to reach the poorest people with other public services;
- continue to have the highest level of political commitment from national governments and multilateral institutions;
- close the funding gap - US$590 million is still required to fund activities in 2011-2012;
- make a donation.
11. Why is so much attention paid to polio and not other diseases?
Polio is one of the few diseases that can be completely eradicated, as was the case with smallpox. By eradicating polio, we will benefit children around the world, and no child will ever have to suffer the pain of paralysis caused by polio. Most diseases, such as HIV and malaria, cannot be eradicated because the ability to do so does not yet exist. Polio does not have a direct host (i.e. it does not affect animals, and its virus cannot exist in animals, in the same way that malaria exists in mosquitoes, for example); There is a safe and effective vaccine to protect children from polio; it does not survive for long periods of time in the environment and although it is contagious, its infectious period is relatively short. Polio eradication efforts are also helping to strengthen routine health care. Polio eradication efforts have created an active polio surveillance network in all countries, which is now integrating other diseases, including measles. Polio eradication infrastructure is also used to provide other health services, such as the distribution of deworming tablets, vitamin A and mosquito nets.
Oral polio vaccine (OPV)
12. Why are children given oral polio vaccine?
The polio vaccine is the only means of protection against polio, a paralyzing disease for which there is no cure. It is important to ensure that every child under 5 years of age is immunized against polio. The oral polio vaccine is safe and effective, and because it is administered orally, it can be given by volunteers.
13. Does oral polio vaccine have any side effects?
Oral polio vaccine (OPV) is one of the safest vaccines ever created. It is so safe that it can be given to sick children and newborns. It is used worldwide to protect children from polio and has saved at least 5 million children from permanent paralysis caused by polio. In extremely rare cases, the attenuated virus in the oral polio vaccine may mutate and become virulent again. The risk of getting polio for children is much higher than the risk of side effects from using the polio vaccine.
14. What are the teachings of Islam regarding the polio vaccine?
Oral polio vaccine (OPV) is safe and has been declared halal by Islamic leaders around the world - Grand Sheikh Tantawi of Al-Azhar University, the Grand Mufti of Saudi Arabia and the Indonesian Ulema Council.
15. Is it safe to give multiple doses of OPV to children?
Yes, it is safe to give children repeated doses of polio vaccine. This vaccine is intended to be given multiple times to provide complete protection. In tropical regions, several doses of polio vaccine, sometimes more than 10, must be used to ensure complete protection for a child. This vaccine is safe for all children. Each additional dose further strengthens the child's immunity against polio.
16. How many doses of OPV does a child need to provide protection?
The oral vaccine must be given several times to be fully effective. The number of doses needed to immunize a child depends entirely on the child's health and nutritional status and the number of other viruses to which he has been exposed. Until a child is fully immunized, he or she is at risk of contracting polio. This highlights the need to immunize all children during each round of national immunization days. The polio virus can be hidden in the body of every unvaccinated child.
17. Should a child be given OPV during polio campaigns and routine immunization?
Yes. Oral polio vaccine (OPV) is safe and effective, and each additional dose means the child receives additional protection against polio. Multiple doses of OPV are required to achieve complete immunity against polio. If the child has received the vaccine previously, additional doses received during national or subnational immunization days will provide valuable additional immunity against polio.
18. Is OPV safe for sick children and newborns?
Yes. Oral polio vaccine is safe for sick children. In fact, it is extremely important to vaccinate sick children and newborns in campaigns because their level of immunity is lower than that of other children. All sick children and newborns should be vaccinated in upcoming campaigns to give them the protection they need from polio.
19. Why do some industrialized countries use a different polio vaccine than developing countries?
All but two countries in the world (Sweden and Iceland) used oral polio vaccine (OPV) to eradicate polio and continued to use OPV generally until the late 1990s, when some switched to inactivated polio vaccine due to progress made towards the eventual eradication of polio. (when the risk of wild poliovirus has decreased). Most countries use OPV because it has the unique ability to induce local gut immunity, meaning it can interrupt transmission of wild poliovirus in the natural environment. This is not possible with IPV, an inactivated polio vaccine that stimulates only a very low level of immunity against poliovirus in the intestine, resulting in individual protection against polio, but, unlike OPV, cannot prevent the spread of wild poliovirus.
News September 24, 2021 Poliomyelitis and its prevention
September 24, 2021 Allergies in children: signs, causes, treatment
September 24, 2021 Listen to a child’s heart
News archive
Causes of polio
The disease is caused by the polio virus. There are currently three known serotypes of poliovirus: PV1, PV2 and PV3. The most common serotype is PV1. The PV2 variant was last recorded in 1999, and since 2015 it is considered completely destroyed. The same fate befell serotype PV3, which was last recorded in 2012. In 2019, its complete destruction was announced.
Children from polio-affected countries. Photo: PHIL CDC
Polioviruses are distinguished by their resistance in the external environment. They remain active in water for up to 100 days, and in feces for up to 6 months. Such viruses are not killed by drying and freezing. They are also able to survive in the aggressive environment of the stomach. The poliovirus can be destroyed by heat, ultraviolet light and chemical disinfection.
Why does paralysis occur?
The virus can only reproduce inside a cell.
To do this, it uses the host's genetic apparatus. When a cell's resources are exhausted, viral particles destroy it and then infect new cells. If such a massive proliferation of poliovirus occurs in nerve tissues, then the neurons quickly die. This leads to paralysis and paresis. The likelihood of paralysis increases under the following circumstances:
- neurological diseases, such as hydrocephalus or malformations of the nervous system;
- previous brain surgery;
- congenital or acquired immunodeficiency;
- traumatic brain injuries.
Routes of infection
The source of infection is a sick person. In most cases, the disease is asymptomatic. For every case with a pronounced clinical picture, there are from 100 to 1000 asymptomatic cases in which the pathogen is detected only by laboratory analysis.
The virus is transmitted by the fecal-oral route. You can catch the infection through dirty hands, contaminated food or water. In rare cases, polioviruses are transmitted through respiratory droplets.
With the fecal-oral route of infection, the virus begins to multiply in the lymphoid tissues of the intestine. And in the case of airborne droplets - in the lymphoid tissues of the nasopharynx. The virus then enters the bloodstream and spreads throughout the body.
It is noteworthy that a person becomes contagious even before symptoms develop (if this is a case with clinical manifestations). Viral particles are detected in nasal mucus within 36 hours after infection, and in feces after 3 days.
A person is most contagious during the first week of illness. Polioviruses are released from the nasopharynx within a week, and from the intestines - up to 6 weeks.
Immunity after illness
After an illness or vaccination, a person develops immunity to poliovirus.
However, such protection is type-specific - it is formed for a specific type of virus. Thus, a person can become ill again if they are infected a second time with a poliovirus of a different serotype. Antibodies to the polio virus are also passed from mother to child. If a woman is sick during pregnancy, the antibodies penetrate through the placenta into the baby’s bloodstream, where they remain for up to a year.
Today, polio does not occur in pregnant women. There were many such cases before mass vaccination. In pregnant women, polio progressed longer and more severely. The disease increased the risk of congenital anomalies and intrauterine fetal death.
Features of vaccination during an epidemic
Modern mothers often ask pediatricians whether a vaccinated child can get polio during an epidemic, and what consequences he faces. Every mother wants only health for her child.
Relatives and the state are jointly responsible for the emergence of an epidemiological situation. Doctors do not particularly conduct an explanatory policy, and parents, due to a lack of understanding of the severity of the disease, often refuse to vaccinate their children for prevention. In addition, the quality of the proposed vaccine is unknown.
Popular Compliance with safety and hygiene rules against leptospirosis
If your child is not vaccinated promptly, he or she may become infected with the polio virus and also put other children at risk of infection, since the disease can often be asymptomatic. What to do if an epidemiological situation arises? Let's consider the algorithm of correct actions:
1. First of all, the child must be given an inactivated vaccine, if it has not been given previously;
2. If the child has already been vaccinated, then during the epidemic, in order not to become infected with polio again, he is given a live oral vaccine in the form of drops. Vaccination is carried out three times with an interval of one month between each;
3. If vaccination is carried out for the first time, then it is necessary to administer the inactivated vaccine to the child two times in a row (with a one-month break between them). During this time, the body will have time to develop immunity to the live polio virus. The third vaccination is droplets.
Classification
There are several forms of polio depending on the type of disease, its severity and course. By type, polio is typical (with damage to the central nervous system) and atypical (without damage to the central nervous system).
Typical forms of polio are non-paralytic and paralytic. The non-paralytic form is the meningeal form, which occurs as meningitis.
The paralytic form can come in several forms:
- spinal (damage to the spinal cord) - flaccid paralysis of the limbs, torso and neck;
- bulbar (damage to the cranial nerves) - disturbances in speech, breathing, swallowing and cardiac activity;
- pontine (damage to the brain stem) - complete or partial impairment of facial expressions;
- cerebral - proceeds as encephalitis;
- mixed - a combination of different variants of the paralytic form of polio.
Non-paralytic poliomyelitis can occur in two forms:
- inapparent form - carriage of the virus without any symptoms;
- abortive (or visceral) form - nonspecific general symptoms characteristic of most viral diseases (fever, intoxication, headache and others).
Poliomyelitis can be mild, moderate or severe in severity. The criteria for the degree of the disease are intoxication and the severity of motor disorders.
The course of the disease can be smooth (asymptomatic or symptoms characteristic only of polio) and non-smooth. In the latter case, these may be complications, exacerbations of chronic infections, or the emergence of new infections due to polio.
Paralysis of the right leg after suffering from polio. Photo: PHIL CDC
Symptoms of polio
The incubation period for polio most often lasts from 7 to 12 days. However, it can last up to 35 days. Clinical manifestations usually occur at 2-6 weeks of illness. After the illness, the patient recovers from 1 month to several years, depending on the severity of the pathology.
In most cases, polio is asymptomatic. Clinical manifestations are observed in 20-25%² of patients. The following syndromes may occur:
- intoxication - accompanied by increased body temperature, general weakness and loss of appetite;
- meningeal syndrome - headaches and photophobia;
- indigestion—nausea, vomiting, bowel dysfunction (diarrhea or constipation);
- neurological syndrome - paresis or paralysis.
Let's take a closer look at the symptoms of various forms of polio.
Figure 1. Poliomyelitis: general information. Image: VectorMine/Depositphotos
Inapparent form and virus carriage
With this variant of polio, there are no symptoms. In this case, the virus usually multiplies in the intestines. Such patients are diagnosed only in foci of infection. If a person is asymptomatic and there is no growth of specific antibodies to the poliovirus, then a virus carrier is established.
Abortive form
Approximately 80% of cases of the disease occur in the abortive form. It is also called minor disease. As a rule, symptoms last from 2 to 5 days. These are fever, sore throat, general weakness and digestive disorders. Since there are no specific symptoms, a diagnosis can only be made through a virological study of the lesions.
In the abortive form of polio, the nervous system is not affected. The prognosis for this type of infection is favorable.
Meningeal form
This variant of polio occurs as serous meningitis, an inflammatory disease of the brain. The symptoms of intoxication in this case are more pronounced than in the abortive form.
This variant of polio is characterized by headache, nausea and vomiting accompanied by high body temperature. The patient experiences increased sweating (especially of the head), increased heart rate (tachycardia) and low blood pressure.
The meningeal form of the disease can occur in one wave (up to 65% of cases) or in two waves. In a single-wave course, meningeal symptoms occur at the onset of the disease, after 1-3 days. With a two-wave course, symptoms of the abortive form of poliomyelitis initially appear, and after 1-4 days - meningeal.
This type of polio occurs without paralysis or paresis. Possible excessive tension in the neck muscles. The prognosis is usually favorable. Recovery occurs within 3-4 weeks.
Paralytic form
Paralysis and paresis with polio occur in 0.1-1% of cases. This form of the disease occurs in 4 stages:
- preparalytic - from 1 to 6 days;
- paralytic - 1-3 days;
- restorative - up to 3 years;
- residual - more than 3 years.
The disease begins with a preparalytic period, which is characterized by symptoms of abortive poliomyelitis. This is an increase in body temperature, intoxication, cough, runny nose and sore throat. High temperature can occur in waves with periodic normalization for 1-2 days. In rare cases, intestinal symptoms develop.
Symptoms such as headache, lethargy, photophobia, increased sweating and tearfulness indicate the first damage to the nervous system. At the end of the preparalytic period, general symptoms subside and the patient's condition improves. However, muscle pain increases. This indicates the transition of the disease to the paralytic stage.
The paralytic period is characterized by the appearance of paralysis and paresis. It is believed that if the virus has destroyed 40-70% of the motor neurons of the spinal cord, paresis develops. Damage to more than 75% of neurons leads to paralysis. As a rule, paralytic symptoms increase within 3 days. The muscles most often involved are the leg muscles. The patient partially or completely loses the ability to bend and straighten his limbs.
The degree of damage and severity of symptoms in the paralytic form of poliomyelitis depends on the level of damage to the nervous system. If the poliovirus infects nerve tissue at the thoracic level, the regulation of the respiratory muscles is disrupted until breathing stops completely, which leads to the death of the patient.
Iron lungs
In 1904, the German surgeon Ernst Ferdinand Sauerbruch was the first in the world to use large iron chambers with variable air pressure for operations.
This is a kind of analogue of modern artificial lung ventilation devices. When the pressure in the chamber dropped, air was forced into the lungs. As the pressure increased, air came out of the lungs. A person in such a chamber could maintain breathing if his lungs failed. Since 1928, “iron lungs” began to be used for patients with polio. During epidemics, thousands of sick children lived in such devices, whose neurons responsible for respiratory function were damaged.
In many patients, breathing was never restored. They had to live in such devices for years and decades. In 2008, Dianne Odell, who had been in such a device since 1950, died due to a power outage.
Today there are still people living in such devices. One of these is Paul Alexander, who contracted polio in 1952. For almost 70 years he was chained to an iron apparatus, and this did not prevent him from receiving a lawyer’s education and working to this day.
Iron lung device for polio patients. Photo: PHIL CDC
The clinical picture of the paralytic period depends on which part of the central nervous system is affected by the virus:
- Spinal shape. This is the most common form of paralytic polio, occurring in 95% of cases. It is characterized by paralysis of the legs, and less often of the arms, torso and neck. If the patient experiences shortness of breath and limited mobility of the chest, this is a sign of damage to the diaphragm and intercostal muscles.
- Bulbar form. This variant of the disease is characterized by impaired swallowing and speech. In the bulbar form, the centers responsible for breathing and cardiac activity are often affected, which leads to corresponding consequences. Most often this is arrhythmic breathing, irregular heart rhythm, decreased blood pressure, even collapse. In mild cases, recovery occurs from the 2nd week. In severe cases, death is possible within the first week of the disease.
- Pontine form. It is extremely rare and is characterized by paresis and facial paralysis. It becomes asymmetrical - the corners of the mouth are lowered, and the nasolabial fold is smoothed.
- Mixed form. Most often this is a combination of bulbar and spinal forms. The cause of death in such patients is respiratory failure. As a rule, in young children, bulbospinal forms of poliomyelitis are more complicated.
- Cerebral form. This is the rarest variant of the paralytic form. Clinical picture of the type of encephalitis. Patients develop convulsions, impaired consciousness and spastic paralysis. Poliomyelitis can be diagnosed in this case only through virological testing.
After the paralytic stage, a recovery period begins, which lasts from 3 months to 2-3 years. During the first 6 months, muscle innervation improves, and the body intensively recovers from illness. Then, over the course of another 2 years, the remaining nerve cells develop slightly. This helps partially compensate for the loss of function caused by paralysis.
If during the first 6 months after recovery muscle function is not restored, then they speak of a residual (residual) period. Paralysis persists, leading to muscle atrophy, joint stiffness, and curvature of the bones and spine.
Poliomyelitis in children
There are non-paralytic (asymptomatic, abortive, mepingeal) and paralytic forms of polio, which are characterized by the manifestation of different symptoms.
Non-paralytic forms
The non-hardware, or asymptomatic , form of polio does not manifest itself clinically. Children with the inapparant form are dangerous to others; they excrete the polio virus in their feces, and they have a high concentration of specific antibodies in their blood. It should be emphasized that the frequency of the inapparent form is quite high.
The abortive form has a number of symptoms: acute onset with elevated body temperature, catarrhal symptoms, moderate headache. Gastrointestinal disorders (abdominal pain, nausea, frequent, loose stools) are often observed, especially in young children. This form proceeds favorably, usually after 3-7 days recovery occurs. It should be noted that the diagnosis of inapparant and abortive forms of polio is quite difficult and is carried out only on the basis of epidemiological and laboratory data.
The meningeal form of polio occurs as serous meningitis: it has an acute onset, high body temperature, severe headache, and repeated vomiting. Patients experience stiff neck muscles, Brudzinski's and Kernig's symptoms, spontaneous pain in the arms, legs and back, skin hyperesthesia, positive symptoms of tension in the roots and nerve trunks (Nery, Lasègue, Wasserman's symptoms), pain on palpation along the nerve trunks, in some muscle groups may experience fasciculations (short-term involuntary contraction of muscle fibers, which manifest themselves in the form of subcutaneous flutter).
With a lumbar puncture, a clear, colorless fluid is usually obtained; the pressure may be increased, cytosis, and the amount of glucose in the cerebrospinal fluid may be increased. The course of the meningeal form of poliomyelitis is usually favorable, recovery occurs in 3-4 weeks, normalization of the cerebrospinal fluid begins in the 3rd week.
Paralytic forms
Among the paralytic forms of poliomyelitis, spinal, pontine, bulbar, and bulbospinal are distinguished.
The spinal form of poliomyelitis is divided into 4 periods: preparalytic, paralytic, restorative, residual. The clinical picture of the disease develops after an incubation period that lasts 10 days. During this period, the polio virus is present in the body and can be detected in fecal matter before the first symptoms of the disease. The onset of the disease is acute, the temperature rises to 38-40 ° C, often with a twofold rise over the course of 5-7 days. Patients are bothered by headaches, frequent vomiting, pain in the limbs and back. Neurological symptoms often appear on the second rise in temperature: stiff neck (resistance to performing passive movements), positive Brudzinski, Ksrnig symptoms, tension in the roots and nerve trunks. Fasciculations may be observed in individual muscle groups, and sweating is pronounced. The duration of the preparalytic period is 6 days, but in some patients paralysis develops from a clear preparalytic period. Paralysis usually occurs at the end of the febrile period or in the first hours after the temperature drops. The spinal form can be localized in the cervical, thoracic, and lumbar regions, depending on which part of the spinal cord the motor cells of the anterior horns are affected. The paralysis is flaccid, marked by hypo- or areflexia; later, from the 2-3rd week, muscle atrophy occurs with a change in electrical excitability (degeneration reaction). The most severe forms are spinal, affecting the diaphragm and respiratory muscles of the chest. Breathing falls on inhalation and rises on exhalation; auxiliary muscles are included in breathing. The duration of the period is several days, sometimes the increase in paralysis occurs within several hours, but it can take up to 2 weeks. The restoration processes of impaired functions begin in the 2nd and 3rd weeks. The most affected muscle groups are involved in the recovery process at a later date; sometimes the pathological process does not reverse, and atrophy increases. Subsequently, joint contracture, trophic disorders, osteoporosis develop, and limbs may lag in growth. The recovery period usually lasts throughout the year, especially active in the first months of the disease, then a period of residual effects begins. In 80-90% of patients with the spinal form of acute polio, there are changes in the cerebrospinal fluid, initially the same as in the meningeal form, and then, in the 2-3rd week, protein-cell dissociation can be observed.
Pontine form of polio. The polio virus infects the nucleus of the facial nerve located in the pons. As a rule, one side suffers. The function of facial muscles is impaired. The eyelids stop closing, it is impossible to wrinkle the forehead or puff out the cheeks. The corner of the mouth becomes motionless, the brow reflex decreases or is lost.
The bulbar form of poliomyelitis occurs with damage to the nuclei of the IX, X, XII cranial nerves, which leads to disorders of swallowing, phonation, and pathological secretion of mucus. A sharp deterioration in the condition of patients is observed with damage to the respiratory and vasomotor centers with disruption of vital functions. Breathing becomes periodic and arrhythmic, then the function of the respiratory center fades, and vasomotor disorders develop. The patient's excitement gives way to somnolence, and a coma occurs. If death does not occur, then after 2-3 days the process stabilizes, and in the 2-3rd week the recovery period begins.
In the bulbospinal form of poliomyelitis , the clinical picture shows a combination of bulbar symptoms with paresis and paralysis of the muscles of the trunk and limbs. A condition in which, along with damage to the respiratory center, paresis and paralysis of the respiratory muscles develops is especially dangerous for the patient’s life. When the nucleus of the facial nerve, located in the pons of the brain, is damaged, the pontine form develops. The latter is characterized by paralysis of facial muscles in the absence of lacrimation, taste disturbances, and impaired pain sensitivity. An increase in body temperature, the development of intoxication often does not occur, and there is a complete or partial loss of facial movements on one half of the face. The palpebral fissure does not close, the corner of the mouth is lowered. Sometimes there is a bilateral lesion with varying depths of disturbance of the facial muscles. During an epidemic, the initial formation of the process can develop in the pontospinal form, which is characterized by a severe course in combination with damage to the respiratory, vasomotor centers and paralysis of the respiratory muscles.
When to see a doctor
In Russia, no cases of polio have been registered for several years. Asymptomatic cases and abortive forms usually remain undiagnosed. Poliomyelitis is suspected when flaccid paralysis or paresis occurs. The epidemiological situation and vaccination with oral (live) vaccines are also taken into account, since polio can be vaccine-associated.
In very rare cases, live polio vaccine occurs. Photo: PHIL CDC
Complications of polio
As a rule, complications occur in severe forms of the disease. These are cases where poliovirus attacks the muscles of the diaphragm. The movement of the chest is impaired, which can lead to the development of pneumonia. Against this background, areas of collapse of the lung - atelectasis - often form. And if the lung is damaged, the pathogen can enter the bloodstream, which can lead to sepsis.
The most common complication of polio is irreversible paralysis, which occurs in 0.1-0.5% of patients. The child may have permanent facial paralysis or lameness.
Consequences of polio in children. Photo: PHIL CDC
The consequences of polio for adults are less dangerous. As a rule, adults tolerate the infection much easier. The exception is for people with weakened immune systems, such as HIV-infected people. Persistent neurological impairment in adults is very rare.
Post-polio syndrome
According to statistics, in approximately 20-30% of patients, after a long residual period (10 years or more), symptoms of muscle weakness increase. Previously functional muscles begin to weaken and lose their functions. This phenomenon is known as post-polio syndrome. The medical literature describes cases in which symptoms of post-polio syndrome developed 30 years after the acute illness.
How to stop transmission of the virus
The polio virus is widespread everywhere. Poliomyelitis occurs more often in children than in adults. Cases of morbidity are reported from time to time in different parts of the world. Before prevention, which consisted of universal immunization of the population against polio, the disease systematically made itself known through epidemic outbreaks.
Poliomyelitis is seasonal (autumn-summer), like most intestinal infections, and in warm countries, episodes of infection occur throughout the year. In the fifties of the twentieth century, mass vaccination began, as a result, the incidence rate decreased significantly, and then completely disappeared. The circulation of wild strains has also stopped, and today only isolated cases of infection are recorded in the world.
Mass vaccination is the only measure to stop the transmission of the virus in society. In addition to using preventive methods, you can avoid infection if you limit contact with a child who has just been vaccinated for two to three weeks, maximum for a month and a half, by which time he will stop releasing a certain amount of pathogens into the environment. Particularly concerned parents can take a polio antibody test to check the effect of the vaccine.
There is no effective cure for polio; vaccination is the only way to avoid the disease. The vaccine is relatively safe, does not cause complications and allows the formation of collective immunity. In addition, the presence of provoking factors, such as living in unsanitary conditions, a poor diet, failure to comply with hygiene rules, and so on, should be excluded. After vaccination, you may feel slightly unwell, but not always.
Diagnosis of polio
Poliomyelitis can be suspected if there are characteristic symptoms (in the case of a symptomatic form) taking into account the epidemiological history. In particular, the doctor is interested in the following information:
- contact with a polio patient;
- contact with a person who has been vaccinated with a live vaccine within the last 2 months;
- visiting a country where polio outbreaks have been reported.
The doctor also checks the patient’s vaccine status - whether he was vaccinated correctly (whether all the necessary vaccinations were done) and what kind of vaccine it was (live or inactivated). Then laboratory and instrumental diagnostics are carried out.
Laboratory diagnostics
Laboratory diagnostic methods for suspected polio include:
- Blood analysis. There is an increase in the number of leukocytes and an increase in the erythrocyte sedimentation rate (ESR).
- Lumbar puncture. A sample of cerebrospinal fluid (CSF) is taken from the patient using a needle. It is then tested for the presence of lymphocytes, protein and other markers.
- Polymerase chain reaction (PCR). Samples of cerebrospinal fluid, feces, and nasopharyngeal swabs are tested for the presence of viral particles. This is done using PCR, which determines the presence of the viral genome in the samples.
- Serological studies. The patient's blood or cerebrospinal fluid is tested for the presence of antibodies to poliovirus. Such a study is carried out several times, since it is necessary to evaluate the dynamics of the growth of G3 type immunoglobulins.
Instrumental diagnostics
To assess the condition of the muscles and spinal cord in polio, the following instrumental studies are carried out:
- Magnetic resonance imaging of the spinal cord. It is carried out during the recovery phase to assess the extent of damage after the acute period.
- Electromyography. This is a diagnostic method that can be used to assess the condition of muscles and nerve fibers. It can be carried out already on the first day after the onset of symptoms.
Differential diagnosis
If polio is suspected, it is extremely important to carry out a differential diagnosis, since different forms of the disease resemble the course of other pathologies.
- Abortive form. Reminiscent of ARVI or infection with enteroviruses, rotaviruses and other viral infections.
- Meningeal form. During the examination, meningitis is excluded. Severe pain is one of the characteristic signs of the meningeal form.
- Spinal shape. It is necessary to exclude a number of diseases of the musculoskeletal system.
- Paralysis due to polio. In this case, it is necessary to exclude tick-borne encephalitis and polyradiculoneuritis³.
Treatment of polio
No antiviral drugs have yet been developed for polio. Therefore, there is no specific treatment. Existing therapy is aimed at eliminating the symptoms of the disease and restoring the functions of the musculoskeletal system and respiratory organs.
For all forms of polio in children and adults, patients must be hospitalized. A person needs to be isolated while they are infectious. In addition, regardless of the form of the disease, a person needs to be examined, since the disease can occur in waves (first the symptoms of the abortive form, and then the paralytic form).
To strengthen the immune system during illness, drugs with interferon and interferon inducers are used (including available antiviral drugs, such as ribavirin). To restore normal levels of immunoglobulins, preparative immunoglobulins are prescribed. During treatment of paralytic forms of the disease, strict adherence to bed rest is important.
If the respiratory muscles are affected, then a decision is made to transfer the patient to artificial ventilation (ALV). If swallowing is impaired, feeding is carried out through a tube.
Depending on the symptoms and severity of treatment, the patient is also prescribed other drugs. For example, these are non-steroidal anti-inflammatory drugs, glucocorticoids, drugs to restore water-salt balance, diuretics (for edema), nootropic drugs, vitamins and others.
Antibiotics for polio
Antibiotics for poliovirus infection are prescribed in two cases:
- Respiratory failure, indications for mechanical ventilation. In such cases, the risk of bacterial complications increases significantly, which requires preventive antibiotic therapy.
- Development of secondary bacterial infection. In some cases, secondary infections (including bacterial) develop against the background of polio. In such cases, antibiotics are prescribed.
After the acute phase of the disease, a recovery period begins, the duration of which depends on the severity of polio. At this stage, the patient takes vitamin and mineral complexes, as well as drugs that strengthen the nervous system. Preparations with phosphorus and potassium improve muscle condition. Physiotherapeutic procedures are also carried out, for example, electrophoresis, ultra-high frequency therapy, paraffin therapy and others.
During the recovery period, physical therapy and therapeutic massage are prescribed. However, such measures can be resorted to only after the symptoms of intoxication have been completely eliminated.
Prognosis and prevention
With inapparant and abortive forms of the disease, the prognosis is favorable. However, even an asymptomatic course of the disease does not guarantee the absence of post-polio syndrome. After 10-40 years, such people may develop symptoms of muscle weakness and even paralysis.
As for paralytic forms of polio, prognosis depends on the degree of damage to the nervous system. In approximately 1 in 200 cases, the patient will experience paralysis for life. This is mainly paralysis of the legs. Severe forms of polio result in death in 60% of cases due to breathing problems.
Poliomyelitis is a disease against which specific prevention has been developed. This is a vaccination that is included in the vaccination calendar.
Bulbar form
Pediatricians consider bulbar polio to be one of the most severe forms of polio. It proceeds very aggressively:
- With it, poor mobility of the soft palate is observed;
- When drinking liquid, the baby may choke or it may leak through the nose;
- Mucus collects in the respiratory tract;
- The swallowing reflex decreases;
- Hoarseness of voice appears;
- The nuclei of the cranial nerves are affected;
- There is an excited state, a pathological rhythm of the respiratory system;
- Hyperthermia.
With this form of the disease, death is possible on the first or second day. Significant changes can also affect the cardiovascular system. Increased blood pressure, cardiac dysfunction, myocardial dystrophy, gastric distension and bleeding in the gastrointestinal tract are observed.
Popular Prevention and treatment of viral hepatitis B disease
How is polio transmitted?
When infected with the virus, symptoms of polio in children may not be expressed. Why can a child get polio? There are several infection options:
- By airborne droplets. Infection occurs through breathing when the polio virus enters the lungs in suspension;
- By water. When drinking untreated water, the virus can enter the body;
- Contact-household way. With this method, a child becomes infected when he eats food from the same plate with a contact person;
- By nutritional route. Unwashed fruits and berries are eaten.
Vaccination
Large-scale vaccination has helped stop the spread of polio, but outbreaks of the disease still occur in poor countries.
Photo: Wikipedia (Public Domain) Vaccination against polio has been carried out since the 50s of the last century. Two types of vaccines are used:
- Oral polio vaccine (OPV). This is a live vaccine with a weakened virus that is dropped into the mouth. OPV is used to control disease outbreaks and for routine immunization.
- Inactivated polio vaccine (IPV). This is an injectable vaccine used for routine immunization.
Vaccine-associated polio
Live polio vaccines are considered safe for children.
However, in very rare cases (1 time in 2.5-3 million), weakened vaccine viruses can cause a disease called vaccine-associated polio (VAP). VAP often occurs when the child has an inadequate immune status. Also, the cause of such a disease can be mutations of viruses at the stage of their cultivation during vaccine production. Weakened viruses may develop virulent properties.
The course of VAP is similar to that of a disease caused by a “wild” strain of the virus.
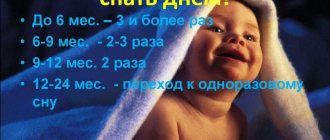
In Russia, as part of the national calendar of preventive vaccinations, polio vaccination for children under 1 year of age is carried out three times - at 3, 4.5 and 6 months4. The first 2 vaccinations are given with an inactivated vaccine to completely eliminate the risk of VAP. OPV is given at 6 months. Then AFP booster vaccination is given at 18, 20 months and 14 years.
Polio
22.Sep.2021
Poliomyelitis is a highly infectious disease. It affects the nervous system and can lead to general paralysis in a matter of hours. The virus is transmitted from person to person, mainly through the fecal-oral route or, less commonly, through some common carrier of infection (for example, contaminated water or food) and multiplies in the intestines. The first symptoms are fever, fatigue, headache, vomiting, neck stiffness and pain in the limbs. One in 200 cases of infection results in permanent paralysis (usually of the legs). 5-10% of such paralyzed people die due to the onset of paralysis of the respiratory muscles.
Polio mainly affects children under 5 years of age. As long as there is at least one infected child in the world, children in all countries are at risk of contracting polio. Failure to eradicate polio from these remaining persistent foci could result in up to 200,000 new cases of the disease occurring annually worldwide within 10 years.
The only protection is timely vaccination. Therefore, parents who care about the healthy future of their child should think about the need for vaccination against polio. Currently, two types of polio vaccines are used: an inactivated (non-live) vaccine, which is administered by injection; and a live vaccine, which contains weakened live viruses. This vaccine is given in the mouth. In Russia, vaccinations against polio are mandatory and are included in the National Calendar of Preventive Vaccinations. All children in the first year of life are subject to vaccination against polio, starting from 3 months with an interval of 6 weeks (further at 4.5 and 6 months). Subsequent vaccinations (re-vaccinations) are carried out at 18, 20 months and 14 years. Before vaccination, a pediatrician must conduct an examination and give permission for vaccination.
Children under 5 years of age are subject to an additional single immunization against polio:
- from families of refugees and internally displaced persons;
- from families of nomadic population groups;
- from families arriving from polio-affected countries;
- have no information about preventive vaccinations against polio;
Additional immunization of children against polio is carried out regardless of the date of arrival without preliminary research.
N. Artyukh, epidemiologist, Nyagan City Children's Clinic
Sources
1. World Health Organization.
Poliomyelitis // Newsletters. — 2021. https://www.who.int/ru/news-room/fact-sheets/detail/poliomyelitis/ 2. What is Polio? // Centers for Disease Control and Prevention. — 2021. https://www.cdc.gov/polio/what-is-polio/index.htm/
3. Samarina V. N., Sorokina O. A. Children's infectious diseases. For doctors of all specialties. — 4th ed., rev. and additional - St. Petersburg, M.: Nevsky Dialect-Binom, 2011. - 336 p.
4. Order of the Ministry of Health No. 125n. “On approval of the national calendar of preventive vaccinations and the calendar of preventive vaccinations for epidemic indications.” garant.ru (March 21, 2014). Date accessed: May 28, 2021.