Pediatrician, physiotherapist, head of the pediatric medical department
Neonatal jaundice is a change in the color of the skin, conjunctiva and sclera (whites of the eyes) in newborns to a yellowish tint due to increased levels of bilirubin (a pigment that is formed when hemoglobin breaks down) in the blood plasma during the newborn period. Neonatal jaundice is usually mild and transient. However, it is important to monitor newborns with severe jaundice or whose jaundice does not resolve naturally, as this may lead to long-term negative consequences. Severe neonatal hyperbilirubinemia is associated with a neurological dysfunction known as bilirubin-induced neurological dysfunction (BIND). In severe hyperbilirubinemia, unconjugated bilirubin crosses the blood-brain barrier, binds to the basal ganglia and brainstem nuclei, leading to acute bilirubin encephalopathy, or progresses to permanent neurological dysfunction that manifests as cerebral palsy, seizures, buckling, and sensorineural hearing loss.
What is the nature of jaundice in newborns?
Jaundice or, scientifically speaking, unconjugated hyperbilirubinemia in newborns occurs due to physiological or pathological reasons. More than 75% of cases of neonatal jaundice are due to physiological reasons. Physiological jaundice is also called non-pathological jaundice because it is mild and disappears spontaneously. This occurs due to the peculiarities in the metabolism of bilirubin in the neonatal period. Increased bilirubin load in newborns occurs due to its increased production, which is caused by a higher mass of red blood cells (RBCs) with a decrease in the duration of their existence in newborns. At the same time, a newborn’s liver is still very inactive, and it processes water-soluble bilirubin into conjugated bilirubin, which is water-insoluble, 100 times slower than in an adult.
Physiological jaundice usually occurs between days 2 and 4 of life, peaks between days 4 and 5, and resolves within 2 to 3 weeks. Physiological jaundice never occurs in the first 24 hours of a newborn's life.
How to speed up the process
According to Dr. Komarovsky, treatment for jaundice in newborns is normally not required, and it is enough to wait until it goes away on its own. Mom shouldn't worry too much about this. But if you want to help your baby’s body, you can use simple tips:
- Milk. Breastfeeding slows down the primary processing of bilirubin, prolonging jaundice. This occurs due to the composition of breast milk. But at the same time, it is the enzymes that it contains that accelerate the process of normalizing liver function. If you do not stop breastfeeding, the baby will return to its usual color much faster. Therefore, it is important to ensure that the baby does not forget to eat regularly due to the drowsiness that accompanies jaundice.
- Walks. No pills or medications are needed to treat jaundice. Regular sunlight helps destroy bilirubin. Therefore, the baby needs to be taken for walks regularly. If the weather permits, it is advisable to spend as much time as possible outdoors.
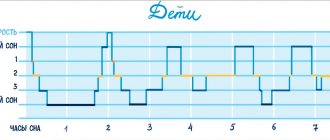
- Lamp. If the weather outside is inclement, then you should not expose your baby to the risk of catching a cold. At home, you can help your baby’s body if he sleeps under a lamp. Light in the blue spectrum works best. But in the absence of special devices, any bright lighting is sufficient. Just don’t forget to protect your baby’s eyes by wearing a blindfold or a hat.
Cramer scale
Normally, the moment when jaundice should subside in newborns under a lamp occurs at the end of the first week of life. Without additional effort, it is enough to wait a couple more days. This completes the natural stage of liver development.
What is pathological jaundice of newborns?
The causes of pathological unconjugated hyperbilirubinemia are also associated with an increase in bilirubin production, a decrease in its excretion from the body and increased blood circulation in the liver and intestines. Pathological jaundice can occur in a newborn in the first 24 hours of life and is characterized by a rapid increase in bilirubin levels of more than 5 mg/dL per day.
The causes of increased bilirubin production in pathological jaundice are immune-mediated hemolysis (destruction of red blood cells) arising due to Rh conflict with the mother, blood group incompatibility or non-immune-mediated causes such as cephalhematoma, defects in red blood cell membranes (hereditary spherocytosis and elliptocytosis), defects enzyme system (glucose-6-phosphate dehydrogenase and pyruvate kinase), which most often affects boys.
Incompatibility of blood groups according to the ABO system occurs in mothers with blood group O, who have IgG antibodies to factors A and B, which penetrate the placenta into the child’s body and cause hemolysis in newborns with blood group A or B. In case of Rh incompatibility, Rh- a negative mother exposed to Rh positive blood from a previous pregnancy becomes sensitized to such blood. This leads to hemolysis in a fetus with Rh-positive blood. To prevent Rh conflicts, anti-D gamma globulin is currently used, which reduces the incidence of hemolysis.
Decreased bilirubin clearance is also observed with hereditary diseases such as Crigler-Najjar and Gilbert syndrome, as well as with diabetes in the mother or congenital hypothyroidism in the baby. For Crigler-Najjar syndrome, newborns may require liver transplantation or long-term use of phototherapy. In Gilbert syndrome, a mutation of the UGT1A1 gene is observed, causing unconjugated hyperbilirubinemia. Gilbert syndrome is usually diagnosed during adolescence, although the first manifestations may occur as early as the neonatal period. It can be diagnosed using genetic testing.
Phototherapy for newborns - what is it?
After a child is born, his body adapts to completely different environmental conditions and undergoes many changes. One of the adaptation mechanisms is physiological jaundice of newborns. In the intrauterine life of a child, his blood contains much more red blood cells than an adult.
This is due to the fact that it receives oxygen by transporting it from the maternal blood through the umbilical cord, and for sufficient saturation it requires a large amount of hemoglobin, which is part of the red blood cells, because it is hemoglobin that carries oxygen to organs and tissues.
After the birth of a child, his body no longer needs such a large number of red blood cells, they are destroyed, releasing fetal hemoglobin, which in turn is destroyed and releases bilirubin, and a large amount of free bilirubin turns the mucous membranes and skin yellow.
Physiological jaundice usually appears on days 3–4 of life and goes away on its own after 2–3 weeks.
Bilirubin is a toxic substance. The body tries to remove it by binding it to the protein albumin.
But if there is significantly more bilirubin than albumin, it affects the nervous system, causing “kernicterus.”
In addition to physiological jaundice, there are pathological forms: conjugative hereditary jaundice, hemolytic disease of newborns, infectious-toxic hepatic jaundice.
One of the most effective methods of reducing bilirubin toxicity is light therapy, or phototherapy.
Phototherapy is one of the physiotherapy procedures based on the therapeutic effects of the ultraviolet spectrum of sunlight with a wavelength of 400–550 nm.
Under the influence of a light wave of the required range, bilirubin is converted into an isomer, which the newborn’s body is able to excrete with physiological waste, which reduces the level of bilirubin in the blood and protects the body from its toxic effects.
Technique of the procedure
A completely undressed child is placed in an incubator, his eyes are covered with special glasses to protect him from ultraviolet radiation, and the boys’ genitals are covered with light-proof fabric. A thick, light-proof gauze dressing is often used.
Ultraviolet lamps are installed at a distance of about 50 cm from the child. Moreover, the combination of four ultraviolet lamps with two fluorescent lamps turned out to be more effective, but the therapeutic effect comes only from the ultraviolet source.
During the procedure, the maximum break can last from two to four hours in a row. In cases of a pronounced increase in bilirubin, light therapy is carried out in a continuous course.
The course lasts on average 96 hours.
Every hour the baby is in the incubator, it is necessary to change the position of his body - on his back, on his stomach, on his side, and measure his body temperature every 2 hours to avoid overheating.
It is worth knowing that during phototherapy, the daily volume of fluid required for a child should exceed the physiological need by 10–20%.
It is necessary to take the baby’s blood for biochemical analysis daily (and if there is a threat of encephalopathy, every 6 hours); this is the only method that serves as a criterion for the effectiveness of the treatment.
Indications for phototherapy
Indications for phototherapy in newborns are:
- the risk of developing hyperbilirubinemia in a child identified during pregnancy;
- morphofunctional immaturity of the child;
- the presence of extensive hemorrhages and hematomas;
- newborns requiring resuscitation;
- identified high risk of developing a hereditary form of hemolytic anemia;
- physiological jaundice of newborns;
- hemolytic disease of newborns with blood group incompatibility - as the main method of treatment;
- hemolytic disease of newborns with Rh conflict - as an additional method of treatment after blood transfusion to prevent a re-rise in bilirubin levels;
- preparation for replacement blood transfusion and rehabilitation after surgery;
- an increase in bilirubin of more than 5 µmol/l per hour for full-term infants and more than 4 µmol/l per hour for premature infants.
Indications for newborns in the first week of life depending on weight and bilirubin level (*):
- body weight less than 1.5 kg, bilirubin level from 85 to 140 µmol/l;
- body weight up to 2 kg, bilirubin level from 140 to 200 µmol/l;
- body weight up to 2.5 kg, bilirubin level from 190 to 240 µmol/l;
- body weight more than 2.5 kg, bilirubin level – 255–295 µmol/l.
Jaundice due to breastfeeding disorders
A decrease in intestinal activity in a newborn leads to increased enterohepatic circulation. Jaundice in the absence or insufficient breastfeeding and intestinal obstruction are common conditions associated with increased enterohepatic circulation, which leads to unconjugated hyperbilirubinemia. Non-breastfeeding jaundice occurs in the first week of life and is caused by insufficient breast milk intake, which leads to dehydration and sometimes high sodium levels in the baby. Lack of breastfeeding leads to decreased intestinal motility and decreased excretion of bilirubin in feces or meconium. This jaundice occurs at the end of the first week, peaks in the second, and usually resolves by 12 weeks of age.
Jaundice resulting from impaired bile transport
Conjugated hyperbilirubinemia is always a pathology and occurs due to defects in the formation or transport of bile caused by mechanical obstructions to its outflow or systemic diseases that can affect the liver. Such conditions include biliary atresia, common bile duct cysts, idiopathic neonatal hepatitis, and Alagille syndrome. Congenital metabolic disorders such as galactosemia, tyrosinemia, antitrypsin-1 deficiency also manifest themselves in the form of conjugated hyperbilirubinemia. Biliary atresia is the most common cause of conjugated neonatal hyperbilirubinemia. It affects both intrahepatic and extrahepatic bile ducts and usually appears during the first 2–4 weeks of life along with pale stools. Initial diagnosis is by ultrasound, which may show the absence of the gallbladder. Ultrasonography can also detect cysts with normal or dilated intrahepatic bile ducts, or sclerotic ducts in biliary atresia.
Jaundice in adults: causes and treatment
Jaundice in adults is manifested by the appearance of a characteristic shade of the skin, mucous membranes and eyeballs. Such symptoms are explained by excessive concentration of bilirubin in the body. It can be caused by various pathological processes. If bilirubin is not excreted from the body, its content in the blood increases. The most common jaundice is caused by viral infections, that is, hepatitis. Diagnostics, which includes a series of laboratory tests, allows you to determine the type of virus.
Symptoms and causes of the disease
In addition to the yellowness of the skin and eye sclera, other manifestations are observed. This is darkening of urine, loss of appetite, allergic reactions, venous network in the abdomen, nagging pain. A common cause of jaundice is liver disease. Symptoms may vary depending on the nature of the pathology. This could be infection by parasites, neoplasms, complications after surgery, etc.
Types of jaundice
Accurate identification of the cause of jaundice is important for effective treatment.
The conjugation form of the disease is typical for infants. In an adult, it can appear due to congenital anomalies or toxic effects on the body (for example, with long-term use or overdose of medications).
The hemolytic form of jaundice develops as a complication of other diseases, due to the rapid destruction of red blood cells and difficulty in removing bilirubin. For example, this form of jaundice threatens patients with leukemia, anemia, and malaria.
Parenchymal jaundice is characterized by damage to the liver tissue. The functionality of cells and the performance of the liver as a whole are impaired. This form of jaundice can be caused by cirrhosis of the liver or infection with viral hepatitis. Its difference from other types of disease is the formation of spider veins and a reddish tint to the skin.
Obstructive jaundice occurs when the ducts are blocked by stones or a tumor, and the flow of bile is disrupted.
Accurate diagnosis – correct treatment
If clinical symptoms appear, you must immediately consult a doctor to establish an accurate diagnosis, the cause of the pathology and begin treatment. Without timely treatment, the pathological process may become irreversible, and the only chance to save a life will be a liver transplant. The examination plan is drawn up on an individual basis. In most cases, it includes blood biochemistry, bilirubin testing, and liver tests. If a tumor is detected, a biopsy is prescribed. Also, to establish an accurate diagnosis, the doctor may need the results of tests for liver enzymes, as well as other laboratory and instrumental studies.
Treatment is prescribed only after the exact cause of the bilirubin metabolism disorder has been established. In most cases, this is conservative therapy. Surgery is an organ transplant. Drug treatment is aimed at preserving liver function and preventing the development of cirrhosis. If the cause of jaundice is a viral infection, it is important to protect the patient’s environment from infection. The main goal of therapy is to stop the pathological process. With adequate treatment, the liver can subsequently restore its functionality.
An important point in treatment is diet. A diet that makes it possible to reduce the load on the liver, but at the same time contains the necessary amount of nutrients, is developed by the doctor individually for each patient.
Diagnosis of liver function
Total bilirubin
Jaundice due to infectious diseases
Systemic infections such as toxoplasmosis, syphilis, varicella, rubella, cytomegalovirus and herpes simplex, and systemic conditions such as sepsis, shock and birth asphyxia may also present as jaundice caused by conjugated hyperbilirubinemia. Neonatal urinary tract infections and long-term use of parenteral nutrition in preterm infants are also known causes of conjugated hyperbilirubinemia.
How common is jaundice in newborns?
Almost all newborns will have a total bilirubin level above the upper limit of normal for adults and older children of bilirubin of 1.5 mg/dL with less than 5% total conjugated bilirubin. Up to 60% of full-term infants and 80% of newborns at 35 weeks' gestation or more will have jaundice, which occurs when plasma bilirubin levels exceed 5 mg/dL. Neonatal jaundice is more common in people living at high altitudes and in people living around the Mediterranean Sea, especially in Greece.
How is jaundice diagnosed?
Diagnosis of a newborn with jaundice begins with a detailed history, including birth history, family history, and onset of jaundice. A complete examination of the newborn should include general appearance, eye examination, abdominal assessment for hepatomegaly, splenomegaly or ascites, neurological examination and assessment of skin rashes. Bilirubin levels can be assessed using a transcutaneous measurement device or blood draw to determine total serum or plasma bilirubin levels. Transcutaneous measurement reduces the frequency of bilirubin blood tests, but is not possible after phototherapy. In addition, if the transcutaneous bilirubin level is greater than the 95th percentile on the transcutaneous nomogram or the 75% of the total serum bilirubin nomogram for phototherapy, the total serum bilirubin level should be measured.
Ultrasound and additional tests such as antibody titers for infection, urine culture, viral culture, serologic titers, amino acids, and α-antitrypsin phenotype may be added to the list of investigations in the case of a suspected diagnosis of conjugated hyperbilirubinemia.
Laboratory testing of the mother's blood will also be required to distinguish between unconjugated and conjugated jaundice. The American Academy of Pediatrics recommends universal screening of all newborns for jaundice and identification of risk factors for severe hyperbilirubinemia. Major risk factors in newborns over 35 weeks include high bilirubin levels, jaundice observed in the first 24 hours of life, blood type incompatibility, gestational age between 35 and 36 weeks, previous siblings who have received phototherapy, cephalhematoma or significant bruising, absence of breastfeeding feeding and East Asian race. Prematurity is also a known risk factor for the development of severe hyperbilirubinemia.
Minor risk factors include maternal diabetes, polycythemia, male gender, and maternal age over 25 years.
Caring for a premature baby, jaundice, a newborn baby - a neonatologist answers questions
Number of views: 18,079
The patient of a neonatologist is a newborn child. A neonatologist deals with children from the first minutes to the 28th day of life. The very first four weeks are a very important time for every baby. Timely examinations and assistance will enable the child to grow up healthy. Premature babies especially need the help of such a specialist. A neonatologist is a specialist with a special profile. The doctor needs to take a comprehensive approach to the little patient in order to understand what processes are occurring in the child’s body.
On April 12, MamExpert was visited by pediatrician, neonatologist, head of the pediatric department of the Clinical Maternity Hospital of the Minsk Region (premature babies and pathology of newborns), Inna Stanislavovna Valentyukevich. She answered our mothers' questions. We publish questions and answers in this article.
The Clinical Maternity Hospital of the Minsk Region is one of the leading obstetric and gynecological institutions in the Republic of Belarus. Here they provide highly qualified obstetric and gynecological care and provide consultations to children under three years of age. The regional maternity hospital employs professionals who provide specialized specialized medical care to women with the most complex obstetric, gynecological and extragenital pathologies. Doctors use the most modern obstetric technologies and care for babies with extreme low birth weight - from 500 grams.
Question: We are 20 days old and have already encountered constipation. We are mixed fed. I follow a nursing diet. Please tell me why this could have happened and how to deal with it?
Answer: Your problem is called functional constipation, constipation can be organic, when there is a malformation of the gastrointestinal tract, this is only 5%, in the total 95% it is functional in nature, associated with nutrition. In your case, it is associated with the introduction of formula milk and the transfer to mixed feeding; although the milk formula is adapted, it is produced on the basis of cow's milk. Intestinal motor function changes, often as a result of impaired digestion of nutrients - carbohydrates and fats. At the same time, gas formation increases and intestinal motor function decreases, constipation occurs. According to WHO definition, constipation is the presence of stool less than 2 times a week. You need to assess the condition of your child’s abdomen, if it is not enlarged, tense, or painful - expectant management, you can use glycerin suppositories. If there is a problem with bloating, then instead of the standard mixture, you can introduce either an anti-reflux mixture, which contains carob gum and promotes better stool passage, or a sour-milk mixture. If unsuccessful, examine the child for lactase deficiency (stool pH). DO NOT overfeed.
Question: I gave birth at 40.4 weeks, the Apgar scale was 8/8, but the discharge from the maternity hospital included a diagnosis: morphofunctional immaturity. By what criteria is this immaturity determined, since the child is post-term? Height 49, weight 2990.
Answer: Your baby is not post-term. Postmaturity is a diagnosis that is made upon reaching 42 weeks of gestation. There are certain clinical signs of postmaturity. A full-term newborn baby can be mature or immature. Immaturity is determined by clinical criteria for the immaturity of organs and systems, for example, imperfect sucking, which indicates immaturity in the coordination of sucking, swallowing, breathing, immature skin (the child is born in lubricant), a decrease in the child’s general activity and physiological reflexes, immature liver function, which is manifested by prolonged jaundice . Your child cannot be called small for gestational age because he is within the 10-50 percentile of the Fenton physical development curves, and body length is also within the 10-50 percentile. You can also estimate the head circumference.
Question: Is bowel disorder common during teething? Is the course of Linux enough or is this a temporary phenomenon. We are already on day 5, we were prescribed Linex Forte (teeth appeared first).
Answer: Teething is stressful for the baby’s body; this is a period when the child’s immunity decreases and he becomes vulnerable to various infections. As a rule, this is still an infection or, in this case, functional disorders of digestion. Probiotics, which include Linex, will not harm the child, but the benefits are questionable. Prescribing probiotics is not evidence-based medicine, so a 5-day course is sufficient.
Question: If the first child had jaundice right away, will the second have it? The doctor said to immediately warn the second child when giving birth. Did she give birth exactly on time, and why was she born? My husband is 2 blood plus, I am 1 blood plus.
Answer: Jaundice in newborns can be physiological or pathological. Early jaundice or early hyperbilirubinemia are considered pathological jaundices. Often caused by the following reasons: infections, isoimmunization by erythrocyte antigens, in your case the ABO system, in other cases the Rhesus system, Kell and other rare factors, also metabolic features, liver dysfunction and others. You and your husband have a conflict regarding the ABO system of erythrocyte antigens, so jaundice is possible in the next child. There is no prevention.
Question: How long can a child not go to the toilet (generally) after birth?? Is this serious for his body??
Answer: The baby's meconium, or first stool, should pass within the first 48 hours. The frequency of stool in a child 1 month of age is variable and ranges from 1 to 10 times a day when breastfed. According to WHO definition, constipation is the presence of stool less than 2 times a week. If the stool does not pass in the first 48 hours, the child is in the maternity hospital - the baby will be given an enema and examined for congenital pathologies of the gastrointestinal tract.
Question: We have jaundice, some say that you can’t feed if you have jaundice, others that, on the contrary, you need mother’s milk. Which is correct? And is it possible to be discharged home with jaundice? What bilirubin numbers are critical? I know that you can rent a lamp at home and treat your baby at home, is this option acceptable?
Answer: A child cannot be deprived of breast milk. Even with immune conflicts, a newborn baby does not stop breastfeeding. Jaundice can be physiological and pathological; the bilirubin level after 3 days and up to 14 days up to 250 µmol/l does not require treatment. Treatment of jaundice with a phototherapy lamp at home is prohibited in our country, but allowed in neighboring Russia. In the population, 3-4% of children have jaundice associated with breastfeeding. The period for reaching the maximum bilirubin level is day 15, and can persist for 9 weeks. Treatment is removal from breastfeeding for 48-72 hours (feed with formula or pasteurized breast milk), then breastfeeding again. Caused by the presence of 3-alpha-20-beta pregnanediol in mother's milk, during pasteurization this hormone is destroyed.
Question: The baby was born at 36 weeks. There was neonatal jaundice at birth. Now we are 1.5 months old, we had a biochemical blood test. Total bilirubin 84.59 H; direct bilirubin 15.28 N. There are no visible traces of jaundice on the body. Tell me, how long will this indicator last?
Answer: Your bilirubin numbers do not interfere with your life and growth; less than 80 µmol/l is the invisible spectrum of jaundice. Your condition does not require treatment. Bilirubin levels return to normal by 3-6 months.
Question: I was diagnosed with hypothyroidism during pregnancy. What is the likelihood that this will be passed on to the child? When should a newborn be examined for this problem?
Answer: Your hypothyroidism is acquired. It is inherited and congenital hypothyroidism is diagnosed in the neonatal period. In the maternity hospital, all newborns are screened (blood test) for hypothyroidism.
Question: I heard that now in maternity hospitals they don’t treat babies’ navels, is that true?
Answer: They are not processed only in the delivery room. 2 hours after birth, the baby is admitted to the neonatal ward. The newborn undergoes initial treatment, which is performed by a nurse in the neonatal department. Further, the treatment of the newborn during his stay in the maternity hospital is carried out 2 times a day; at home, the umbilical wound is treated 2 times a day in the morning and evening and after bathing until epithelization (healing).
Question: I was born at 7 months, is the predisposition to premature birth inherited?
Answer: There are many causes of premature birth, the most common of which are infections. The predisposition to premature birth can be inherited. One of the reasons, for example, may be the anatomical structure of the woman’s reproductive system. Genetically, you received one X chromosome from your mother and a second X chromosome from your father, who in turn received it from his mother. If these chromosomes contain a predisposition to premature birth, then it will be passed on to you.
Question: My baby was born at 31 weeks, 6 weeks have already passed, we are at home, everything is fine now. How to understand that the baby is developing correctly?
Answer: You will assess physical development using Fenton centile tables up to 52 weeks of postnatal age (age after birth), the 52 week field according to WHO centile tables for corrected age (the difference between the passport age and the missing ones up to 40 weeks of gestation, in your case 9 weeks) . The pediatric neurologist will also evaluate neurological development at corrected age. Your baby is now 37 weeks old and has not yet reached her due date. Your child's development will be assessed monthly by your pediatrician and by a neurologist at the designated periods: 1, 3, 6.9 and 12 months of corrected age.
Question: What are the main rules for caring for a premature baby? We were born at 35 weeks. We are already being discharged home, it is very scary how to care for him: how to put him to bed, what temperature should the room be, how long does a newborn baby need additional warming. And another question about swimming, what should my temperature be, I read that it was 38-39 degrees, but in the maternity hospital they said that it was 37. Which is correct?
Answer: 35-36 weeks is the gestation period, which in the literature is called almost full-term. There is no difference in care between a full-term baby and your baby after leaving the hospital. Swim at a water temperature of 37 degrees 3-4 times a week, daily walks up to 1.5 hours, in spring-summer-autumn 2 times a day. Your newborn baby is thermostable and does not require additional warming compared to a full-term baby. Children with unstable temperatures are not discharged from the maternity hospital.
Question: What are deep and critical prematurity, what are the differences. And what is the difference between small for gestational age and intrauterine growth retardation?
Answer: Prematurity is determined by gestational age: the number of weeks from conception to birth is less than 37 weeks. There is a special cohort of premature infants - these are children with very low body weight - VLBW - body weight less than 1500 g and with extremely low body weight - ELBW - less than 1000 g. There are no other criteria for the classification of prematurity, the terms deep and critical prematurity are not used. Intrauterine growth retardation is a condition treated by obstetricians and gynecologists, and small for gestational age is the result of intrauterine growth retardation. This is a neonatal diagnosis. The newborn may be small for gestational age, small for gestational age, and small in head circumference for gestational age according to the Fenton centile curves of physical development (less than the 10th percentile). These children need to be prescribed specialized products for premature and low birth weight babies. They have a higher risk of developing metabolic syndrome in adulthood, as well as in adolescence and even childhood.
Question: When can you start placing your baby on his tummy, and for how long?
Answer: Even a newborn baby can lie on his tummy immediately after birth. The baby is placed on the mother's chest on her tummy. The time of lying on the stomach is not limited to 10-15 minutes; the child can lie on his stomach from feeding to feeding. In the first month of life, a newborn should not sleep on his stomach at night, this is to prevent sudden death syndrome.
Question: How to properly feed a premature baby after discharge from the hospital?
Answer: After discharge from the hospital, premature babies need to be prescribed specialized products, such as breast milk fortifiers or specially adapted formulas (pre-1). The lower the gestation, the longer children need to be prescribed such products. This is due to the increased need for protein in premature infants. Protein is the main factor that is necessary for the growth of the brain of a premature baby and to ensure its catch-up growth. Brain growth directly determines neurological development and intelligence. The protein requirement for a premature infant after 36 weeks of postconceptual age (gestational age + passport age) is 3 g/kg per day. This need can be met during breastfeeding only with the use of breast milk fortifiers, and during artificial feeding - with the use of special adapted formulas for premature babies. Fortifiers are breast milk enhancers - special additives that contain protein, vitamins and minerals necessary to meet the needs for macro and micronutrients in premature infants. Calculation of nutrition for premature infants is made solely on the basis of protein requirements; it should be done by your pediatrician; adequate protein supply is monitored by assessing physical development (Fenton tables) and biochemical monitoring (as indicated). The abolition of specialized nutrition is carried out gradually, as a rule, after the introduction of complementary foods.
Question: We were born at 34 weeks and hemorrhagic disease of the newborn appeared on the 2-3rd day. Injected konakeon. Immediately and then again, a few weeks later. Please tell me, how can it still manifest itself in later life? Now we are 3 years old.
Answer: No, this will not manifest itself in any way in your future life, you had a deficiency of vitamin K, which you were replenished with high-quality real vitamin K. You were treated very correctly and you are no longer in danger of vitamin K deficiency.
Question: Tell me, how is an umbilical hernia treated? I read that you can glue a coin to your belly button.
Answer: An umbilical hernia does not pose a threat to the health of your child; these hernias are not strangulated and often go away on their own as the muscles of the anterior abdominal wall develop and strengthen. If the umbilical hernia remains, further surgical treatment is necessary. There is no need to apply a coin; you can use a regular patch, but not constantly, so as not to cause skin irritation. There is also a special patch for umbilical hernias in pharmacies.
Question: Tell me what to do? We started giving Lactazar on IV, a low-lactose mixture (we didn’t give it at night, only during the day). We are tormented wildly by colic: there is no sleep or rest for the baby. They recommended Kuplaton - I started giving it. I've been giving it for two days now. But! Today I leaked a lot after eating, and yesterday the stool was half perfect, and the other half was diarrhea. There are a few lumps of the mixture, but in insignificant quantities. The tummy rumbles even during feeding, everything shoots inside, we spin, arch, push, then, if it can, it farts a couple of times and falls asleep. Then everything repeats again. I put it on my stomach, give it a massage, and give it water. Is it the mixture that doesn’t suit us that well or the colic that’s so intense? It’s just that if you have colic, then it’s clear that time will help us. What if it's a mixture? That needs to be changed! I really don’t want to switch to lactose-free, because... lactose is necessary.
Answer: Your diagnosis is lactase deficiency. Stool with lactase deficiency has a sour odor and is divided into fractions, the liquid part is separate, the mushy part is separate. Abdominal bloating is pronounced. Lactosar (lactase) is an enzyme that is added ONLY to breast milk; it does not need to be added to a low-lactose formula. A low-lactose formula, of course, has advantages over a lactose-free one, but if the clinical symptoms are pronounced and there is no increase in body weight, then it is worth switching to a lactose-free formula for a short period of time, then gradually replacing some of the feedings, and then all of them with low-lactose. Use cuplaton or simethicone (disflatil, espumizan) at every feeding. It is necessary to determine the pH of the stool. Don't overfeed. Try changing the mixture to a mixture from another manufacturer, also low-lactose (lactose-free). You need to consult a gastroenterologist
Was this information interesting and useful for you? Please share your opinion!
comments powered by HyperComments
How is jaundice treated?
To prevent acute bilirubin encephalopathy and kernicterus, severe hyperbilirubinemia is treated with phototherapy, intravenous immunoglobulin, or exchange transfusion. There are nomograms for determining bilirubin levels at which phototherapy and replacement blood transfusion are indicated.
Phototherapy is initiated taking into account risk factors and serum bilirubin levels on a nomogram. Bilirubin optimally absorbs light in the blue-green range (460 to 490 nm) and is either photoisomerized and excreted in bile or converted to lumirubin and excreted in urine. During phototherapy, the newborn's eyes should be protected and as much of the body's surface area should be illuminated as possible. It is important to maintain hydration and urine output because most bilirubin is excreted in the urine as lumirubin. The use of phototherapy is not indicated for conjugated hyperbilirubinemia and may result in “bronze baby syndrome” with grayish-brown skin discoloration.
After cessation of phototherapy, there is an increase in total serum bilirubin levels, known as “reverse bilirubin.” The level of "reverse bilirubin" is usually lower than the level at the beginning of phototherapy and does not require restarting phototherapy.
Intravenous immunoglobulin is recommended if bilirubin levels increase as a result of isoimmune hemolysis despite phototherapy. Intravenous immunoglobin is started when bilirubin levels are between 2 and 3 mg/dL.
Replacement blood transfusion is indicated if there is a risk of neurological dysfunction, either with or without phototherapy. It is used to remove bilirubin from the bloodstream and, in isoimmune hemolysis, also removes circulating antibodies and sensitized red blood cells. Blood transfusions are performed in neonatal or pediatric intensive care units. A double exchange blood transfusion (from 160 to 180 ml/kg) is performed to replace the newborn’s blood. Phototherapy should be restarted and continued after blood transfusion until bilirubin reaches a safe level.
Phototherapy as a method of treating jaundice
Yellowing of the face in the first month of a baby’s life is far from the norm, as many people think. If the jaundice is severe and the bilirubin level is significantly higher than normal, treatment cannot be avoided. There are different methods: taking medications for the liver, sorbents that remove toxins, transfusion of blood components. However, the simplest and most effective way to combat jaundice is phototherapy.
Phototherapy belongs to the category of physiotherapeutic procedures. It is based on the healing properties of UV rays, simulating sunlight with a certain wavelength (in the range of 400-550 nm).
Ultraviolet light, coming into contact with the baby’s skin, neutralizes bilirubin by converting it into an isomer, after which it is easily excreted from the body along with feces and urine. A special photo lamp is used for treatment. The most effective is considered to be a combination of 4 ultraviolet and 2 daylight lamps.
Important! High bilirubin causes intoxication of the body. Infants with jaundice often have no appetite, do not gain weight well, and sleep a lot
If the concentration of bilirubin is not reduced in a timely manner, this can lead to damage to the brain and nervous system (bilirubin encephalopathy).
Phototherapy is based on the effect of ultraviolet lamps on the skin of patients. Such light waves convert the dangerous form of bilirubin into its isomers, which are excreted from the child’s body in feces and urine. The procedure reduces the quantitative indicators of the substance in the blood and prevents the development of a number of complications. The effectiveness of the manipulation is explained by the following points:
- as a result of the oxidation of indirect bilirubin under the influence of UV rays, the formation of biliverdin, mono- and dipyroles occurs, which dissolve in water and are excreted in urine and feces;
- configurational changes occur in the molecules of the indirect fraction of bilirubin, and isomers that are harmless to the body are formed, which again easily dissolve in water;
- Structural changes occur in bilirubin molecules, resulting in the formation of lumirubin. The latter is eliminated from the baby’s body within a few hours.
Experts have found that the phototherapy procedure for neonatal jaundice will produce the maximum effect if the area and intensity of irradiation are as large as possible. Doctors recommend increasing the radiation power to 30 μW/cm2/nm, and also installing the lamps in such a way that ultraviolet radiation hits all parts of the child’s body at the same time.
There are special blankets for phototherapy
Prognosis for jaundice
With timely diagnosis and treatment, the prognosis is positive. In patients with delayed treatment, brain damage is a serious complication. Until now, many doctors (and parents) do not fully understand that jaundice (or as it is sometimes disparagingly called “jaundice”) in newborns is not a benign disease, and requires close attention. The fact is that jaundice in a newborn is a serious disease that can cause irreversible brain damage. All physicians caring for newborns should be aware of this fact. Although many conditions that cause jaundice cannot be immediately diagnosed, the key to preventing complications is to educate parents. Parents should be informed by nurses, pediatricians, obstetricians and the attending physician that if the child's skin, stool or urine color changes, the child should be examined immediately at the clinic. Today, there are smartphone apps that help parents identify jaundice. The main thing is to ensure that the baby is examined in a clinic to rule out any malignant cause of jaundice. Only through the cooperation of parents and doctors can the incidence of jaundice in newborns be reduced.