Causes of mononucleosis
Mononucleosis is caused by a type of herpes virus (Epstein-Barr virus). The route of transmission of infection is airborne droplets.
. The disease does not pose an epidemic threat. The virus quickly dies in the external environment. But it is present in saliva. A child who puts various objects into his mouth can become infected, especially if he is in a group of children in which there is a carrier of the infection. Therefore, outbreaks of mononucleosis sometimes occur in kindergartens.
Family foci of the disease are also recorded. Emphasizing this feature, mononucleosis is called the “kissing disease.” Most often it affects children aged from one to 10 years. The second peak in incidence occurs in adolescence. By the time they reach adulthood, most people are immune to mononucleosis.
Symptoms of mononucleosis
The incubation period of mononucleosis is on average 7-10 days, the maximum duration is 21 days.
Most often, the disease begins acutely, with a rise in temperature. If the temperature does not rise immediately, it usually occurs towards the end of the first week of illness. During the course of illness, the temperature may rise several times. It decreases gradually. In the evening, a slight increase in temperature may be observed for quite a long time. In some cases, no increase in temperature is observed.
Other symptoms may also be present in both pronounced and vague forms.
The acute period of the disease usually lasts 2-3 weeks. The recovery process can take quite a long time (up to several months). Swelling of the lymph nodes and a slight increase in the size of the liver and spleen persist the longest.
The main symptoms of mononucleosis:
Temperature increase
Mononucleosis is characterized by an increase in temperature to 38°C and above. A rise in temperature is accompanied by chills, body aches, and headache.
Enlarged lymph nodes
First of all, swelling of the cervical lymph nodes is detected. Sometimes axillary, inguinal and other groups of nodes increase.
Redness of the tonsils
There is redness and enlargement of the palatine tonsils. Quite often the whole complex of symptoms of angina appears.
Stuffy nose
The nose is stuffy, but there is no discharge from the nasal passages (no runny nose).
More about the symptom
Enlarged liver and spleen
With mononucleosis, an increase in the size of the liver and spleen is observed (reaches a maximum on the 4th – 10th day, but can manifest itself from the first days of the disease).
Rash
Various types of rashes may appear. The rash disappears after a few days, leaving no traces.
More about the symptom
Infectious mononucleosis (Filatov's disease, glandular fever)
HIV
Herpes
Encephalitis
46335 08 October
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Infectious mononucleosis: causes, symptoms, diagnosis and treatment methods.
Definition
Infectious mononucleosis is a viral disease in which fever develops, the liver and spleen, lymph nodes become enlarged, and the larynx and pharynx are affected. Changes characteristic only of this pathology (the appearance of atypical mononuclear cells, lymphocytosis) are recorded in the blood. In some cases, infectious mononucleosis has a chronic course; in some conditions, the clinical picture is erased, which significantly complicates the diagnosis and making a correct diagnosis.
Causes of infectious mononucleosis
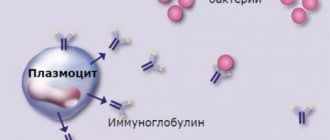
The disease is caused by viruses of the herpesvirus family; the most common pathogen is Epstein-Barr virus (EBV, or human herpes virus type 4). Most people experience it in a mild clinical form in childhood and adolescence, which is confirmed by blood tests for the content of immunoglobulins, which are produced in response to viruses entering the human body: according to statistics, 9 out of 10 adults have positive blood tests for the DNA of this virus.
Routes of transmission of the virus that causes infectious mononucleosis:
- Airborne.
- Contact and household (including sexual).
- Parenteral - during blood transfusion, organ and tissue transplantation during the 6 months preceding the disease.
Predisposing factors for the development of the disease include conditions such as decreased immunity, long-term illnesses or exacerbation of chronic pathologies, unfavorable psycho-emotional and environmental conditions.
Classification of the disease
There is no single generally accepted classification of infectious mononucleosis. For the convenience of formulating a diagnosis, the following divisions of pathology into groups are used:
By pathogen:
- Epstein–Barr virus (EBV).
- Cytomegalovirus.
- Herpes virus types 6 and 7 (HV6, HV7).
- Adenovirus.
- Immunodeficiency virus.
- Toxoplasma gondii (toxoplasma).
Type:
- Typical - a clinical picture characteristic of mononucleosis and pathognomonic (characteristic only for this disease) changes in blood tests.
- Atypical – erased clinical picture, asymptomatic course.
By duration:
- Acute infectious mononucleosis – manifestations of the disease are recorded within no more than 3 months.
- Prolonged course (3–6 months).
- Recurrent course - symptoms of the pathology reappear 1 month or less after the illness.
- Chronic – symptoms persist for more than 6 months.
There are also mild, moderate and severe forms of infectious mononucleosis.
Separately, they note how the disease itself proceeds - with or without complications (for example, with the addition of another viral or bacterial infection), with or without exacerbation of chronic diseases, with the presence or absence of relapses of infectious mononucleosis. Symptoms of infectious mononucleosis
After the Epstein-Barr virus has been introduced into the body, no symptoms arise for a month or a month and a half; this period is called the incubation period. Then the patient begins to experience weakness, increased fatigue, and a feeling of general malaise, which are characteristic of any viral infection. Over the course of a week and a half, all these symptoms gradually decrease. Then, against the background of a seemingly complete recovery, severe sore throat, high fever, weakness, and swollen lymph nodes occur. These symptoms can last for several weeks, and malaise and weakness can last for more than a month. The clinical picture (pain in the throat when swallowing, swollen lymph nodes) is almost identical to that of angina. To make a diagnosis of infectious mononucleosis, a blood test is prescribed, which reveals changes that are unique to this disease. In 10% of patients during this period, a rash appears on the body (its presence or absence does not have any prognostic significance). Due to the enlargement of the liver and spleen, there may be a feeling of discomfort in the abdomen and subcostal areas.
Diagnosis of infectious mononucleosis
The doctor first collects anamnesis and conducts a visual examination of the patient. Upon examination, attention is drawn to enlarged groups of lymph nodes (in severe cases, not only the cervical group, but even internal lymph nodes), hyperemia (redness) of the pharynx, enlargement of the spleen and liver, which the doctor detects by palpation and percussion of the abdomen.
The Epstein-Barr virus infects B-lymphocytes (a type of leukocyte - white blood cell responsible for immunity, in particular, producing antibodies), in response, cells characteristic only of such a lesion and called “atypical mononuclear cells” appear in the blood, and the total number lymphocytes predominate over the number of other leukocytes, there may be an increase or decrease in the total number of white blood cells, a decrease in granulocytes (a subgroup of leukocytes, within which there are specific granules where substances for the implementation of immunity are produced). Granulocytes include, for example, neutrophils, eosinophils, and basophils. All these changes characteristic of infectious mononucleosis are detected during a clinical blood test.
Methods for diagnosing mononucleosis
Symptoms of mononucleosis are not specific. Therefore, diagnosis is based primarily on laboratory data. The necessary studies are combined in the profile “Diagnostics of infectious mononucleosis”.
General blood analysis
A complete blood count for mononucleosis usually shows an increase in the number of leukocytes and ESR. Characterized by a significant increase in lymphocytes and monocytes, together these varieties can account for up to 80-90% of the total number of leukocytes. The main symptom of mononucleosis is an increase in the number of specific cells - atypical mononuclear cells (which are altered lymphocytes) to a level of over 10%. However, they are detected no earlier than on the 5th day from the onset of the disease.
More information about the diagnostic method
Blood chemistry
Mononucleosis can manifest itself in the results of a biochemical blood test in the form of a two- or three-fold increase in the activity of ALT and AST. When the skin turns yellow (jaundice), bilirubin increases.
More information about the diagnostic method
Serological blood test
Using serological analysis, specific antibodies to the causative agent of mononucleosis, the Epstein-Barr virus, can be detected.
More information about the diagnostic method
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Treatment methods for mononucleosis
Treatment of mononucleosis in children is carried out by a pediatrician. In acute cases of the disease, you should call a doctor at home.
There are no specific treatments for mononucleosis. Antiviral drugs, corticosteroids and immunomodulators are prescribed only for severe cases of the disease. Antibiotics are used in case of bacterial infection.
Treatment of mononucleosis is carried out according to a scheme common to many acute respiratory viral infections.
Drink plenty of fluids
To reduce intoxication of the body, you need plenty of warm drink.
Symptomatic treatment
At temperatures above 38.5°C, antipyretic drugs are used. If symptoms of tonsillitis occur, antiseptics are prescribed. Gargling is recommended.
Diet correction
Since mononucleosis can occur with liver damage, a diet limiting fatty, spicy and fried foods is recommended (table No. 5).
Taking vitamin supplements
For mononucleosis, vitamin therapy (vitamins B, C and P) is indicated.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
Complications of infectious mononucleosis in children
With timely diagnosis and treatment, complications of infectious mononucleosis do not occur so often. However, the most common among them is liver inflammation , which can cause jaundice in children. In very rare cases, rupture of the spleen occurs - this is the most dangerous consequence of mononucleosis, which sometimes turns fatal.
When a child has had mononucleosis, his immunity remains weakened for about a year. Therefore, during this period it will be effective to do routine vaccinations after an illness and, if possible, limit the child’s contact with a large number of people, as well as refrain from traveling to places with an unusual climate.
The most insidious feature of mononucleosis is that the mononucleosis virus is oncogenic , i.e. it can have a stimulating effect on the development of cancer. Therefore, it is very important to re-take a blood test after recovery in order to track how the blood composition is being restored.
To prevent these complications, if there are obvious symptoms of mononucleosis in a child, you need to consult a doctor, who, in the case of an acute form of the disease, will ensure hospitalization at the SM-Clinic hospital. Our doctors will quickly diagnose, prescribe treatment and make every effort to ensure that the child recovers as quickly as possible.
Sources:
- A. V. Razgulyaeva, O. P. Ukhanova, S. M. Bezrodnova. Modern ideas about the etiology, pathogenesis, clinic and treatment of infectious mononucleosis in children // Bulletin of the Stavropol State University, 2012, No. 78(1).
- I. A. Zaitseva, S. A. Khmilevskaya, I. A. Berezhnova. Infectious mononucleosis in children // Children's infections, 2004, No. 3.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.