Features of newborn skin
- the skin of a newborn is very thin and delicate, it is three times thinner than the skin of an adult, and its outer layer contains actually one thin layer of cells;
- it is susceptible to irritation and infection, because the ratio of the baby’s skin area to its weight is three times greater than that of an adult, and the blood supply to the skin is 1.5 times higher than that of an adult;
- water and minerals are very intensively released from the skin of a newborn baby;
- the intensity of a baby’s skin respiration is 8 times stronger than that of an adult: he literally “breathes through his skin”; however, when dirt appears on the baby’s skin, the child is deprived of this opportunity;
- infant skin is easily injured;
- the protective functions of the skin of a newborn baby are reduced due to the fact that the mechanism for producing fats in it has not yet been developed, as a result of which the sebaceous and sweat glands almost do not work;
- The baby’s skin has a very high absorption capacity, and during the inflammatory process it increases significantly; for this reason, intoxication of the newborn’s body occurs very quickly;
- The melanin content in infant skin is very low, so it is vulnerable to ultraviolet rays;
Why do newborns' skin peel?
Because due to its thin structure, a baby’s skin loses moisture very quickly and dries out even with the slightest increase in temperature. If your baby overheats (during the summer months or in a too warm room), his skin quickly becomes covered with “islands” of prickly heat - a pink rash.
Features of the basic functions of the skin in children.
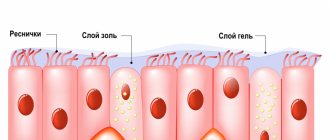
In children, especially young children, the protective function of the skin is low due to the fact that the epidermis has a thin stratum corneum, keratinization is weak, and the connection between the epidermis and the dermis is not strong enough. The dermis has poorly developed connective tissue. Due to insufficient development of glands, the skin surface is drier, and its reaction is close to neutral; local immunity is not mature enough.
The pigment-forming function of the skin is reduced, despite the large number of melanocytes, due to their weak stimulation. Such skin is practically defenseless against UV rays.
The resorption function of the skin in children is increased due to the thinness and friability of the stratum corneum, as well as the abundant blood supply. Therefore, during external treatment, toxic or hormonal ointments can have a pronounced systemic effect.
The excretory function of the skin associated with sweating is imperfect, although the sweat glands are well formed at the time of birth.
The thermoregulatory function of the skin in children is reduced. During the first months of life, heat transfer dominates over heat production due to the relatively large surface of the body, rich blood supply to the skin, significant direct evaporation, and imperfection of the center of temperature regulation. As a result, the child can easily overheat or hypothermia, which leads to the need to create an optimal temperature regime for him.
Ensuring optimal ambient temperature, along with hygienic procedures, is one of the most important conditions for proper skin care of a newborn. This is due to the fact that infant skin is not yet able to cope with thermoregulation, that is, maintain a constant body temperature when the ambient temperature changes. Therefore, in the room where the child is located, it is necessary to maintain a constant temperature of about 22 ° C. Both hypothermia and overheating are equally undesirable for the child (if overheated, in particular, prickly heat may develop).
The respiratory function of the skin in children is 8 times stronger than in adults, due to the thin layer of the epidermis and the rich blood capillary network. Contamination of the skin and lubricating large areas of it with various ointments and creams disrupts the process of skin respiration, which negatively affects the child’s well-being.
The synthetic function of the skin in childhood is fully realized from the age of 3-4 weeks. Under the influence of natural or artificial ultraviolet radiation, vitamin D3 is synthesized in the skin, the deficiency of which leads to the development of rickets.
The skin as a sensory organ functions well from birth. Irritation of the skin is associated with the identification of almost all reflexes of the newborn. Due to insufficient differentiation of the organs of vision and hearing in the first month of life, the child recognizes his mother through tactile perception. At the same time, excessive skin irritation (for example, wet and dirty diapers) can cause anxiety in the newborn, disrupting his sleep and appetite.
In general, the skin of children, especially during the first year of life, is very sensitive to infection, chemical and physical irritants, the influence of atmospheric factors, overheating and hypothermia, is less protected from the penetration of chemical substances into it, and is easily macerated. The anatomical and physiological characteristics of the skin dictate the need for careful hygiene, gentle temperature conditions, prohibition of the use of irritating and toxic substances, etc.
Let's touch on some rules for caring for a newborn's skin. Maintenance is important to ensure a feeling of comfort and create a barrier to the penetration of germs.
Washing in the morning, as well as bathing, should be done daily. In the morning, just wipe the child’s face with a clean cotton swab dipped in warm boiled water. Bathing is the most important general hygiene measure: This procedure not only keeps the body clean, but also stimulates skin functions, blood circulation, strengthens the nervous system and promotes the psychomotor development of the child. You can bathe either in running water or in water with the addition of herbal decoctions - string, nettle, chamomile. The use of detergent is allowed once every two to three days. This should be a mild detergent containing a minimum amount of surfactants (for example, La Cree Cleansing Gel.) The main children's hygiene products used after bathing are baby oil and cream; It is possible to use a special moisturizing lotion (for example, La-Cri emulsion) or baby powder. During the day, it is necessary to ensure that wet and soiled diapers do not come into contact with the baby’s skin for a long time and are replaced in a timely manner. The skin of the buttocks and groin folds requires special care.
. When changing a diaper, you need to wash the baby or wipe it with a special damp cloth, focusing on the folds. Apply cream to clean skin of the buttocks and groin folds, evenly distributing it in a thin layer over the entire area that requires protection from excess moisture and the irritating effects of natural secretions (for example, cream from the “La Cree” series). Pay attention to what components are included in creams intended for children. Substances such as glycerin, beeswax, mineral and castor oil, panthenol, zinc oxide, vitamins A, D, E, C, natural extracts of chamomile, calendula, string, licorice allow the cream not only to perform a protective function, but also to have a protective effect on the skin pronounced antimicrobial and anti-inflammatory effect. In addition, the cream should nourish the skin and have regenerating properties, i.e. promote rapid healing of damaged skin.
Newborn baby skin color
During the first days of life, the skin of a newborn is covered with a special vernix lubricant, similar to cottage cheese: it consists of glycogen, extractives, fat, salts, cholesterol, as well as vitamins and other substances. This layer gradually disappears as a result of drying, using clothes and diapers.
The skin color of a newborn is most often reddish with a bluish tint, while its skin is slightly swollen. You can see a small fuzz of hair on the baby's skin. And the skin of a newborn’s face on the nose and adjacent areas is covered with milia - small white-yellow pimples. After 2-3 days of life, the skin color of a newborn may acquire a yellowish tint: this is due to increased destruction of red blood cells and immaturity of liver enzymes.
Jaundice of newborns
Physiological jaundice of newborns
Transient jaundice is a borderline condition in the neonatal period.
Immediately after the baby is born, excess red blood cells containing fetal hemoglobin are destroyed to form free bilirubin. Due to the temporary immaturity of the liver enzyme glucuronyl transferase and intestinal sterility, the binding of free bilirubin and its excretion from the newborn’s body in feces and urine is reduced. This leads to the accumulation of excess bilirubin in the subcutaneous fat and discoloration of the skin and mucous membranes yellow. Physiological jaundice of newborns develops on days 2-3 after birth, reaching its maximum on days 4-5. The peak concentration of indirect bilirubin averages 77-120 µmol/l; urine and feces are normal in color; the liver and spleen are not enlarged.
With transient jaundice of newborns, a mild degree of jaundice of the skin does not extend below the umbilical line and is detected only with sufficient natural light. With physiological jaundice, the newborn’s well-being is usually not affected, but with significant hyperbilirubinemia, sluggish sucking, lethargy, drowsiness, and vomiting may occur.
In healthy newborns, the occurrence of physiological jaundice is associated with temporary immaturity of liver enzyme systems, and therefore is not considered a pathological condition. When monitoring the child, organizing proper feeding and care, the manifestations of jaundice subside on their own by the age of 2 weeks.
Jaundice of premature newborns is characterized by an earlier onset (1–2 days), reaching a peak of manifestations by the 7th day and subsiding by three weeks of the child’s life. The concentration of indirect bilirubin in the blood of premature infants is higher (137-171 µmol/l), its increase and decrease occurs more slowly. Due to the longer maturation of liver enzyme systems, premature babies are at risk of developing kernicterus and bilirubin intoxication.
Hereditary jaundice
The most common form of hereditary conjugative jaundice of newborns is constitutional hyperbilirubinemia (Gilbert's syndrome). This syndrome occurs in the population with a frequency of 2-6%; inherited in an autosomal dominant manner. Gilbert's syndrome is based on a defect in the activity of liver enzyme systems (glucuronyl transferase) and, as a consequence, a violation of the uptake of bilirubin by hepatocytes. Jaundice of newborns with constitutional hyperbilirubinemia occurs without anemia and splenomegaly, with a slight increase in indirect bilirubin.
Hereditary jaundice of newborns in Crigler-Najjar syndrome is associated with very low glucuronyl transferase activity (type II) or its absence (type I). In type I syndrome, newborn jaundice develops already in the first days of life and steadily increases; hyperbilirubinemia reaches 428 µmol/l and higher. The development of kernicterus is typical, and death is possible. Type II syndrome, as a rule, has a benign course: neonatal hyperbilirubinemia is 257-376 µmol/l; Kernicterus rarely develops.
Jaundice due to endocrine pathology
Usually occurs in children with congenital hypothyroidism due to a deficiency of thyroid hormones, which disrupts the maturation of the enzyme glucuronosyltransferase, the processes of conjugation and excretion of bilirubin. Jaundice due to hypothyroidism is detected in 50-70% of newborns; appears on the 2-3rd day of life and persists for up to 3-5 months. In addition to jaundice, newborns experience lethargy, pastiness, arterial hypotension, bradycardia, rough voice, and constipation.
Early jaundice can occur in newborns whose mothers suffer from diabetes mellitus due to hypoglycemia and acidosis. It manifests itself as a prolonged icteric syndrome and indirect hyperbilirubinemia.
Jaundice in newborns with asphyxia and birth trauma
Fetal hypoxia and asphyxia of newborns delay the formation of enzyme systems, resulting in hyperbilirubinemia and kernicterus. Various birth injuries (cephalohematomas, intraventricular hemorrhages) can be sources of the formation of indirect bilirubin and its increased penetration into the blood with the development of icteric staining of the skin and mucous membranes. The severity of jaundice in newborns depends on the severity of the hypoxic-asphyxia syndrome and the level of hyperbilirubinemia.
Pregnane jaundice
Aries syndrome, or jaundice of breastfed children, develops in 1-2% of newborns. It can occur in the first week of a child’s life (early jaundice) or on days 7-14 (late jaundice of newborns) and persist for 4-6 weeks. Among the possible causes of pregnane jaundice in newborns is the presence of maternal estrogens in milk, which prevent the binding of bilirubin; unsteady lactation in the mother and relative malnutrition of the child, causing reabsorption of bilirubin in the intestine and its entry into the bloodstream, etc. It is believed that risk factors for jaundice in breastfed newborns are later (after 12 hours of life) passage of meconium, delayed cross-clamping umbilical cord, stimulation of labor. The course of this type of jaundice in newborns is always benign.
Kernicterus and bilirubin encephalopathy
With a progressive increase in the concentration of indirect bilirubin in the blood, it can penetrate the blood-brain barrier and be deposited in the basal ganglia of the brain (kernicterus of newborns), causing the development of a dangerous condition - bilirubin encephalopathy.
At the first stage, the clinical signs of bilirubin intoxication predominate: lethargy, apathy, drowsiness of the child, monotonous cry, wandering eyes, regurgitation, vomiting. Soon, newborns develop classic signs of kernicterus, accompanied by stiff neck, spasticity of the body muscles, periodic agitation, bulging of the large fontanel, extinction of sucking and other reflexes, nystagmus, bradycardia, and convulsions. During this period, which lasts from several days to several weeks, irreversible damage to the central nervous system occurs. Over the next 2-3 months of life, a deceptive improvement is observed in the children’s condition, but already at 3-5 months of life, neurological complications are diagnosed: cerebral palsy, mental retardation, deafness, etc.
Newborn baby skin care
Until the age of six months, the baby must be bathed daily, but you should not leave him in the water for a long time (more than 5-10 minutes). Immediately after bathing, it is necessary to treat the still wet skin of the baby’s face and the scalp of the newborn with special milk or oil, and only then can it be wiped with light blotting touches. The so-called products for “bathing without tears” are not a whim of modern mothers, but an important part of caring for a child’s skin, because by choosing these products, you preserve the lipid barrier in the child’s skin and protect it from serious damage. Shampoo “without tears” for the scalp of a newborn baby should be used no more than 1-2 times a week, and cream-gel should be used for daily bathing.
Expert comment:
Dermatologists try not to prescribe antiseptics, alcohols, urea, and salicylic acid to treat the baby’s skin. After all, all these substances very quickly penetrate the baby’s skin and quickly end up in the bloodstream. Infant dry skin is a normal condition that affects one third of children. Sometimes the skin contains not only peeling, but also microcracks, which are also a normal physiological condition.
Yellow coloring is a sign of jaundice
Yellow skin color in a baby is a sign of jaundice. This is a common and generally harmless condition in newborns that causes their skin, eyes, and sometimes stool to appear yellow.
Jaundice is the result of elevated levels of bilirubin, a yellow-orange substance produced when red blood cells are broken down in the liver.
Jaundice is sometimes a sign of various disorders - from benign to serious, especially if it does not go away in the first weeks after birth or does not occur immediately after birth. For example, mild jaundice may be a sign of benign hereditary Gilbert syndrome. It occurs quite often - in three to five percent of people. In the presence of this syndrome, jaundice occurs during tension, stress, fasting or infectious diseases. Fortunately, it usually does not cause health problems, so treatment is not required.
Yellow skin color in a newborn can signal dangerously high levels of bilirubin, which often leads to serious problems - liver disease, deafness, cerebral palsy and even brain damage. Timely treatment, including phototherapy and/or blood transfusions, usually helps prevent these severe consequences.
But the yellow-orange color of the skin of a newborn baby is not only a sign of jaundice. This may be carotenemia, caused by excess beta-carotene in the blood. The main cause of carotenemia is eating too many carrots, sweet potatoes or pumpkin. Green and yellow vegetables and fruits also sometimes contain high levels of beta-carotene. Even egg yolks and milk are rich in this substance.
The yellow-orange color caused by carotenemia is more noticeable in fair-skinned infants. It is usually more pronounced on parts of the body that sweat actively, such as the palms of the hands, soles of the feet, and the skin around the nose and mouth. The color change is more noticeable under artificial light. Fortunately, carotenemia is safe and usually goes away on its own when high-carotene foods are eliminated from the child's diet.
Newborn skin care: why does it need special care?
Expert comment: First of all, because the skin is very delicate, and as a result of this, various dermatitis often develops on it. In addition, the condition of the child’s skin directly depends on the presence or absence of infectious diseases among parents and caregivers. The risk of infection of the baby's skin is very high, since at birth the child has wound surfaces, and their main focus is concentrated in the umbilical wound. With inadequate care of a child's skin, the pH of which is slightly acidic, its balance quickly shifts to the alkaline side.
When caring, it is necessary to pay special attention to the numerous folds on the skin of a newborn baby, especially if the baby is overweight: after all, infected diaper rash is essentially the result of poor care of the baby, untimely treatment of his skin after contact with urine and feces. Parents should remember that it is in infancy that the immune system is formed and allergic reactions occur. This includes atopic dermatitis, which begins with damage to the skin barrier.
How to properly care for your baby's skin:
- limit contact with biological fluids: feces, urine, sweat, saliva;
- to prevent diaper rash, use zinc-containing products - both under the diaper and for treating skin folds;
- use only those children's cosmetics that soothe the skin and enhance its regeneration;
- choose only hypoallergenic baby skin care products that contain components similar to physiological ones and also soothe the skin and have a mild anti-inflammatory effect;
- Children's cosmetics should be suitable for care from “zero” age.
Children's cosmetics for treatment must exclude harmful components:
- Phthalates are fragrances that dampen the unpleasant odor of the product base associated with a petroleum product. Phthalates can cause asthma, infertility, decreased testosterone concentrations in boys, and delay puberty in girls during puberty. Due to side effects, some types of phthalates are banned in the US and EU countries.
- Parabens are preservatives that prevent the development of microorganisms in cosmetics and, as a result, disrupt the skin microbiome. Parabens may have a weak estrogenic effect, penetrate the skin and accumulate in the body. Subsequently, they can cause the development of breast cancer and miscarriage.
- Surfactants (surfactants) that are responsible for the “foaminess” of shampoos and other detergents. They remove not only dirt and fats, but also the skin’s own lipid layer. These products are especially dangerous for children with atopic dermatitis, as they severely irritate the skin.
What cosmetics should you choose when caring for your baby’s skin:
- with cotton extract, which has protective, softening and nourishing properties;
- with lanolin - a wax of animal origin that preserves the lipid barrier of the skin;
- with panthenol, which restores and moisturizes the skin;
- with wheat proteins, which restore the protective barrier of dry skin in a newborn;
- with soybean oil, which promotes skin regeneration;
- with aloe vera, which stimulates and heals the skin;
- with grape seed oil - a natural antioxidant.
What exactly is needed when treating a newborn’s skin:
- massage oil with a soft and light emollient (a substance that helps soften dry skin in a newborn);
- if deeper hydration is required, a special baby cream will work well - but one that does not leave a wet film on the child’s skin (to avoid this, cotton extract and highly purified lanolin are added to high-quality creams);
- In winter, classic cold creams containing a significant amount of water in oil will help protect the dry skin of a newborn from the effects of various external factors (these creams can also treat the skin of a newborn’s face);
- care when changing a diaper involves the use of a zinc-containing and anti-inflammatory agent.
Conditions and reactions of the skin of newborns and infants. What is important to know and what you should not be afraid of.
Neonatal period – first 28 days
Infancy period – up to 1 year
Birth is the most interesting, beautiful, but often frightening event for parents and newborns themselves. Let's look at the main special conditions and reactions of the skin of newborns and infants so that we can all feel more comfortable about this new life!
What skin conditions can a child have:
1. Original lubricant. A whitish-gray mass covering the skin of a newborn. It is a product of the sebaceous glands mixed with epidermal scales. It looks like the baby is covered in soft cheese. This substance protected his body from getting wet and bacteria, so there was no need to remove it. It will gradually absorb into the skin itself.
2. “Lullaby cap.” Remains of vernix with scales on the head. A condition related to dandruff. It looks as if gray-yellow scale-like crusts are glued to the scalp and hair. They can cover the entire scalp, combining like a real “bonnet.” No correction is required, but it can be gradually removed with a mild shampoo.
3. Primary lanugo hair. Very soft fluff covering the baby's body. They usually fall out before birth, but can remain for up to 1 week after birth. In premature babies, delicate down thickly covers the entire body, but then also falls out.
4. Transient baldness. A frequently occurring phenomenon of postnatal hair change, manifested in the form of areas with their absence or a decrease in density, usually in the back of the head, less often in the frontoparietal. Observed at the age of 3-4 months. No treatment is required, the hair will grow back on its own.
5. Erythrosis. Moderate redness of the skin during the first three days. This is a normal condition and is often followed by peeling of the skin.
6. Skin peeling. Light, flour-like, in the form of delicate grayish scales. May last more than 3 weeks, but resolves on its own. More typical for premature and post-term babies.
7. Yellow line of the abdomen. It appears as a vertical line and looks like a yellow stripe on the stomach. Appears at 3-8 weeks of life and disappears on its own after 2-3 months.
8. Vascular spots (vascular nevus of Unna, “stork bite”, “angel’s kiss”). They may be present on the back of the head, bridge of the nose, forehead, eyelids and, less commonly, lips from birth. There is no need to be afraid of this. They are considered to be vestigial remains of embryonic vessels. They are red-pink spots with unclear boundaries, turning pale or disappearing when pressed. Usually, they gradually resolve on their own during the first years of life.
9. Mongolian spots. Bluish-gray discoloration of the skin in the area of the cross, buttocks, or thighs. It is a variant of benign pigmented intradermal nevi. In brunettes, it is resolved by the age of 3-6 years. In people of the Mongoloid race, they appear in more than 80% of cases and persist for a long time or do not resolve at all.
Next, let's look at the reactions that can occur on the skin of babies:
1. Vascular reactions.
Marbling of the skin. Looks like leaf-shaped spots in shades of purple on the skin. It is considered a normal variant associated with functional atony of venules (outflow vessels) and hypertonicity of arterioles (small blood vessels) during the first three months. In the case of persistent marbling at a later age, consultation with a neurologist is recommended to exclude disturbances in the functioning of the central nervous system and a cardiologist to exclude pathology of the cardiovascular system.
Acrocyanosis. A transient reaction that manifests itself as a change in skin color to shades of blue in areas distant from the heart, such as the palms and soles, and the area around the mouth. May be noticeable in the first 2 days.
Harlequin-type changes. When the child is positioned on his side, the lower part of the body becomes purplish-red, and the upper part becomes lighter. Looks like a “Harlequin costume”. May occur for up to three weeks. Manifestation after 1 month is grounds for consultation with a cardiologist to rule out heart disease.
Transient swelling. They most often occur on the external genitalia and in the lower half of the body. They are considered as a reaction to tissue compression during childbirth, or to hypothermia, and are sometimes associated with transient spasms of the cardiovascular system or urinary system of newborns. They appear in the first few days or up to three weeks and, in the absence of pathology, go away on their own.
2. Reactions to cold and heat.
Heat rash (miliaria). It may appear in case of sudden profuse sweating due to overheating, which is facilitated by imperfect thermoregulation of young children. I would like to note right away that you should not be afraid of her, although sometimes she can have a rather frightening appearance. It appears in the form of red spots, papules (small raised pimples), blisters on the head, neck, torso, and sometimes in folds. When infected with staphylococci, small pustules appear. If it appears, then it is necessary to avoid overheating, provide the child with air baths and carry out the maximum possible ventilation of the rooms where the child is. Sometimes treatment is required in the form of disinfectants and adsorbents in the form of solutions and powders.
Cold panniculitis. Subcutaneous nodes or plaques appear a few hours, less often days, after hypothermia. Most often it appears in the cheek area in the form of dense “lumps.” Usually, it resolves on its own and does not require treatment. Skin protection in cold weather is necessary.
This article gives a general idea of the physiology of infants and newborns and I hope it will be interesting and useful to parents. But, undoubtedly, each specific person and case requires an individual approach, and if there is the slightest doubt about the physiology of the condition, or a lack of understanding of its nature, this should be a reason to contact a specialist.
Marble shade of cobwebs on the skin
If you notice a spiderweb-like pattern on your baby's skin, your baby most likely has the fairly common phenomenon of cutis marmorata, a marbled skin color in newborns that often occurs in children in the first months of life.
The skin takes on a marbled or mottled hue due to the large number of unformed blood vessels located very close to its surface. Some of these vessels narrow, giving the skin a bluish tint, while others widen, hence the reddish color, which is how a network-like pattern appears. It may become more noticeable when the baby is cold and fade as the baby warms up.
The marbled skin color of a child does not pose any threat and disappears on its own when the child gets a little older. There is another, very rare form of this condition called congenital telangiectatic marbled skin (CTMC), in which the marbled meshwork on the skin is more noticeable and does not go away when the child warms up. This condition is more common in children living in cold climates.
Although this phenomenon is usually not dangerous, about half of children with this type of marbled skin also have other skin features, such as port-wine stains and hemangiomas. These babies also have an increased risk of developing problems with their teeth, bones, or eyes. This syndrome usually does not require treatment, and children most often outgrow it by puberty or even earlier.