Causes of diarrhea in a child
Physiological factors
Frequent loose bowel movements caused by damage to the gastrointestinal tract should not be confused with normal feces of the newborn and infancy period.
Babies have pasty or loose stools with a slight sour odor if they are breastfed, and firmer, more viscous stools when formula-fed. The physiological frequency of bowel movements in newborns is up to 8 times a day, which does not belong to the concept of “diarrhea.” Short-term diarrhea occurs when there are errors in the diet - the immediate consumption of large amounts of sweets, fatty or unhealthy foods. Infants experience stomach upset when switching to another formula or when introducing complementary foods. The symptom goes away in a couple of days and is not accompanied by a general deterioration in health. Sometimes diarrhea in a child begins under severe stress, but after eliminating the provoking factor, it immediately disappears.
Intestinal infections
This is the most common cause of bowel problems in children, which is detected in all age groups, but poses the greatest threat to children under 5 years of age. Infectious diarrhea is characterized by an acute, sudden onset and the presence of other signs of poisoning - nausea and vomiting, pain in the abdominal cavity, rumbling and flatulence. According to the etiological principle, intestinal infections are divided into the following groups:
- Viral
. Rotaviruses, noroviruses, and enteroviruses are the main causes of diarrhea in pediatric practice. They cause loose stools, in which mucus is noticeable, with a frequency of up to 15-20 times per day. Sometimes during defecation, watery discharge with a fecal odor is observed, which indicates a severe secretory form of diarrhea. - Bacterial
. With salmonellosis, liquid, foul-smelling green stool is released; with escherichiosis, bright yellow or orange stools are produced; with shigellosis, defecation occurs with a meager volume of mucus mixed with blood, like “rectal spitting.” Cholera is characterized by watery, rice-water-like stools. - Protozoans
. Pediatricians periodically encounter giardiasis, which occurs as typical enteritis or enterocolitis. Less commonly, children develop amebiasis, for which diarrhea “raspberry jelly” is pathognomonic - mucous feces with a large number of blood streaks.
Diarrhea in a child
Food allergies
Allergic enterocolitis in children is manifested by liquid, mucous stool, which may contain food particles. In severe cases of the disease, blood appears in the stool. The intensity of the symptom depends on the amount of allergen eaten and the type of hypersensitivity reaction - diarrhea can occur within a few hours to several days after consuming the allergen. It is associated with respiratory and skin symptoms.
Chronic gastrointestinal diseases
Prolonged diarrhea lasting more than 14 days or occurring with periods of exacerbation and remission is observed in gastroenterological patients. It is more typical for school-age children and is mainly associated with non-infectious inflammatory lesions of the intestines and other digestive organs. This group of pathologies includes:
- Congenital disorders.
Prolonged and repeated diarrhea develops in children suffering from celiac disease and disaccharidase deficiency. It is typical for the patient's condition to worsen after taking the appropriate products. During defecation, copious mushy or liquid foul-smelling masses are released, and there may be particles of undigested food in the stool. - Somatic diseases
. Periodic episodes of diarrhea occur with an inadequate diet and insufficient drug control of chronic pancreatitis, cholecystitis, and hepatitis. Exacerbation occurs after consuming prohibited foods. Loose stools are accompanied by pain in the projection of the affected organ, nausea, and vomiting. - Inflammatory bowel pathologies
. With Crohn's disease, the child complains of repeated loose bowel movements and severe abdominal pain. Sometimes, at the time of defecation, heavy bleeding occurs, scarlet streaks or dark blood clots appear in the stool. With nonspecific ulcerative colitis, diarrhea is scanty, and blood is visible in the stool.
Surgical diseases
Acute appendicitis in pediatric surgery can occur under the guise of a foodborne toxic infection. The child has multiple loose stools without pathological impurities, and this distinguishes the clinical picture of inflammation of the appendix from the “adult” version. Diarrhea is accompanied by refusal to eat, nausea and vomiting, and pain in the abdominal cavity. At the same time, pathognomonic physical symptoms and protective muscle tension are slightly expressed.
Complications of pharmacotherapy
In modern pediatrics, antibiotic-associated diarrhea occurs, and its frequency is maximum in children of the first years of life, which is associated with inferior intestinal microflora. Typically, symptoms of gastrointestinal disorders are provoked by treatment with cephalosporins, tetracyclines, lincosamides and macrolides. The child has stool up to 10-15 times a day. Feces are liquid or foamy, foul-smelling, with a greenish tint.
Diet in children with diarrhea
In the acute phase of the disease, feed your baby only liquid or pureed food. Foods can be chopped or pureed using a blender. It is recommended to serve the meat to the child in the form of puree or baked soufflé.
If possible, limit or completely avoid foods that increase peristalsis. You need to feed your baby less fresh vegetables and dairy products.
If your baby is breastfed, you should continue to breastfeed. In case of diarrhea, you should increase the amount of food you drink, while reducing the portion. The same should be done with a child who is artificially fed.
If you are feeding your baby special baby-approved tea or water, continue. In case of excessive diarrhea or vomiting, the amount of fluid administered should be increased.
Diagnostics
During the examination, the pediatrician carefully collects anamnesis and asks whether there were any patients with similar symptoms in the family or in an organized children's group. To exclude acute surgical pathology, assess nutritional status, degree of dehydration, and perform a physical examination. A number of diagnostic methods are used to determine the cause of diarrhea:
- Ultrasound of the abdominal cavity.
Sonography is a fast and non-invasive method that allows you to exclude urgent surgical conditions and study the structural features of the gastrointestinal tract. During the examination, the doctor can detect chronic inflammatory processes, congenital developmental anomalies, signs of damage to the liver, pancreas and other organs. - X-ray of the gastrointestinal tract.
In case of chronic diarrhea, the gastroenterologist is interested in the condition of the walls of the stomach and intestines, so he prescribes X-rays with barium contrast. Irrigography helps to exclude damage to the colon. - Stool tests.
Typical deviations in the coprogram: the presence of undigested food particles, striated muscle fibers, increased levels of mucus and leukocytes. Stool culture is performed to exclude bacterial intestinal infections. Viral pathogens are identified using stool PCR. - Blood tests.
Clinical and biochemical tests are needed to assess the general condition of the child and diagnose the presence and degree of dehydration. Serological reactions are used to identify infectious pathogens in severe cases and generalization of the disease.
Stool culture
Treatment
Help before diagnosis
If a child has diarrhea, he should be given water regularly to prevent exicosis. Lightly salted boiled water, dried fruit compote, and weak herbal tea are suitable for these purposes. The liquid is given in small portions (1-2 teaspoons) every 5-10 minutes. After loose bowel movements, you should give 50-200 ml of water, depending on age and weight. If you categorically refuse to eat, you cannot force the child to eat.
To quickly remove toxins from the body, you can use enterosorbents. Self-prescribing treatment with antibiotics and other medications is prohibited. If diarrhea in a child is accompanied by blood in the stool, complete refusal of water and food, or a sharp increase in temperature, you need to seek emergency medical help. Another warning sign is sharp abdominal pain, especially in the right side of the abdomen, which may indicate appendicitis.
Conservative therapy
Children with satisfactory general condition are treated on an outpatient basis. The remaining categories of patients are subject to hospitalization in an infectious disease, gastroenterological or surgical hospital. Since acute infectious diarrhea is most common, the main principle of therapy is adequate rehydration. According to the severity of exicosis, it is carried out according to three schemes:
- Plan
A. In the absence of dehydration or mild dehydration, oral rehydration is prescribed with water or special solutions of oral rehydration salt (ORS). The child is given liquid regularly in small sips; after bowel movements, he should drink at least half a glass of water. For breastfed babies, it is recommended to increase the frequency of breastfeeding. - Plan b
. With moderate exicosis, an increased oral water load is provided in the first 4 hours to eliminate pathological losses due to frequent bowel movements. After feeling better, switch to standard maintenance rehydration, as in plan A. - Plan
B. Severe exicosis requires immediate initiation of intravenous infusions of saline solutions. Their volume and electrolyte composition are calculated based on the patient’s weight and blood test results. After removing the child from a serious condition, an oral rehydration method is used.
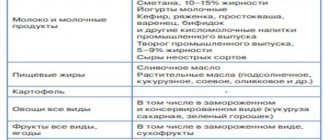
Diet plays an important role. In case of acute diarrhea in the first days, gentle nutrition is necessary - pureed porridge, slimy soups, dry biscuits, a small amount of stewed vegetables. Next, the diet is expanded with lean meat and fermented milk products. For diarrhea due to cholecystitis or pancreatitis, the menu is drawn up taking into account the underlying disease. Bowel disorders due to celiac disease require strict adherence to a gluten-free diet.
Drug treatment is tailored to the cause of diarrhea. For mild and moderate acute intestinal infections, etiotropic treatment is not carried out. However, severe bacterial infections with hemocolitis are an absolute indication for antibiotic therapy. Antibiotics must be prescribed to children suffering from primary and secondary immunodeficiencies and severe concomitant pathologies.
Enterosorbents, antiemetic and antidiarrheal drugs (according to strict indications!) constitute the pathogenetic treatment of diarrheal syndrome. To improve the intestinal microflora, probiotics in combination with prebiotics are recommended for children. Medicines shorten the duration of stool disorders and accelerate the restoration of digestive tract functions in children. For chronic intestinal pathologies, the gastroenterologist must reconsider the treatment regimen.
Norfolk virus diarrhea
Norfolk viruses belong to a separate group of round viruses.
The diseases they cause are widespread throughout the world. In developed countries, they cause 30% of all viral diarrhea. Most children already at an early age suffer from latent or obvious forms of Norfolk virus infection.
Routes of infection
Infection occurs through the consumption of unboiled water and food that has not been heat-treated.
Features of the disease
The mechanism of action of viruses is similar to rotavirus infection. The main changes occur in the small intestine. Norfolk viruses disrupt the structure of the mucous membrane, as a result of which enzyme activity decreases and the absorption of carbohydrates and fats is impaired. After an illness, strong immunity remains. Recurrent disease is caused by other viruses from the Norfolk group.
Course of viral diarrhea
The latent (incubation) period ranges from 1 to 3 days. The disease begins acutely, with the appearance of abdominal pain, nausea and vomiting. Later, loose, watery stools without pathological impurities appear up to 3-5 times a day, infrequent vomiting for 1-2 days. Body temperature rises slightly and not in all children. Symptoms of intoxication are not clearly expressed.
The disease is acute, and recovery occurs in two to three days.
Diagnosis and treatment
Diagnosis is made after a laboratory examination (PCR, ELISA, etc.).
There is no specific treatment that destroys these viruses in the human body. Therefore, the main points of assistance are:
- complete rehydration - feeding the sick person,
- selection of the optimal type of therapeutic nutrition.