What body temperature is considered elevated in a child?
To begin with, it is worth deciding on normal temperature indicators. Body temperature is considered elevated if it:
- above 37.2°C in the armpit and scalp
- above 37.8°C in the oral cavity
- above 38°C in the rectum and auricle.
For babies under one year old, a higher figure will be considered normal - up to 37.4 ° C in the armpit.
During the coronavirus pandemic, these temperature indicators can be considered one of the symptoms of COVID-19. To exclude this infection, an in-person consultation with a doctor is required.
How to measure correctly
Not all parents know how to correctly measure a child’s temperature so that the readings on the thermometer are reliable. Some mothers forcefully try to measure it on a baby who cries and struggles, and this can negatively affect the measurement result.
Measurements are usually taken in the armpit and take about 10 minutes. You can use any thermometer - mercury or electronic.
When measuring temperature with an electronic thermometer, after the sound signal, you need to hold it under your arm for another 3-4 minutes. In this case, its readings will be comparable to mercury.
It is convenient for babies to use infrared thermometers, special pacifiers and test strips. In order for them to show the correct result, it is important to follow the instructions before using them.
Which thermometer is best to use to measure temperature?
There are three types of thermometers used to measure a child's body temperature:
- mercury is the most common thermometer. Its advantage is that such a device measures temperature more accurately than others. The downside is fragility. This is the least preferred way to measure temperature in children. A mercury thermometer is easy to break. The baby may be injured by shrapnel. And mercury is dangerous to health;
- electronic - a simple, modern and convenient thermometer. It is the one that is preferable for children. The downside may be its accuracy. Before using the device for its intended purpose, you should compare its readings with the readings of a mercury thermometer. Take several measurements with both devices on a healthy, adult family member. If the readings differ by no more than 0.1°C, then such a thermometer can be placed in a home medicine cabinet;
- infrared - the advantage of such a thermometer is that it is more accurate than an electronic one. Measures temperature quickly. You don’t need to hold it for a long time, you just need to apply it to the skin for a few seconds. It is very convenient for kids. And also for older children, when you need to measure their temperature while they sleep. The downside is the price - this is the most expensive option. There are different types of infrared thermometers. Some need to be pressed against the skin, others measure temperature at a certain distance from the surface. These thermometers have attachments for measuring temperature in the ear, mouth, and rectum.
For accurate measurements, it is important to use the thermometer correctly. The mercury thermometer must be pressed firmly against the skin. It must be held until the mercury stops rising. Electronic thermometers usually have an audible signal at the end of the measurement. You definitely need to wait for him.
What are the causes of high fever in a child?
There are reasons for increased body temperature that are not related to illness.
1. In babies under one year old, due to imperfections in the thermoregulation system, an increase in body temperature may occur as a response to high ambient temperatures. The autonomic nervous system in children is not fully formed, sweating is not perfect, their body cannot adapt to environmental conditions as well and quickly as in adults. In summer, the reason is hot weather. In winter - excessive amounts of clothing.
To prevent your baby from overheating, you need to:
- monitor your drinking regime. In hot weather, it is recommended to give children boiled water;
- walk in the morning or evening hours. In hot weather, limit your baby’s stay outside;
- avoid open sun. Walk in the shade of buildings and trees;
- dress children according to the weather. Do not wrap your child too tightly in winter. In hot weather, dress your child in single-layer clothing made from natural, breathable fabrics. Cover exposed areas of the body as much as possible to avoid sunburn. Don't forget about hats. Choose a light color for them;
- try, if possible, to avoid or reduce the time of traveling with a child in transport;
- For older children, it is quite possible to organize water procedures in the fresh air.
2. An increase in temperature in a small child may occur as a reaction to vaccination. Typically, such an increase is short-lived - one or two days. The readings on the thermometer, however, do not reach too high numbers - up to 38.5°C. There is nothing wrong with such a reaction to the vaccine. On the contrary, this may indicate that the baby is developing a strong immune system.
Typically, this condition does not require any special actions from parents. Just care and drink. If the child is feeling unwell, the temperature can be brought down in the same way as with any other condition. If the temperature rise lasts for a long time, the numbers on the thermometer are too high, or the baby has other complaints, a pediatrician’s consultation is necessary.
Read more about post-vaccination reactions in children in our article “What can happen to a child after vaccination?”
3. Sometimes an increase in temperature in a child is associated with a disruption of the nervous system. In this case, the temperature remains for a long time, does not reach high numbers and does not affect the general well-being of the child. The reason for this increase in temperature is trauma or previous infections of the brain. For example: concussions, brain contusions, meningitis or encephalitis. This condition requires contacting a pediatrician and neurologist, additional examination and specific treatment.
4. The most common cause of high fever in a baby is infection. We will talk about it in more detail.
Main reasons
A high temperature is not always a runny nose, cough or sore throat. Sometimes it can occur without visible symptoms. An increase in temperature is a normal reaction of a child’s body in response to viruses, bacteria or the development of an inflammatory process. The nervous system can react in this way to the baby's hyperactivity. It can be the body's reaction to pain during teething or injury. The main thing is to understand the reason and, if necessary, provide assistance correctly.
Bacterial infection
Bacteria (staphylococci, pneumococci, streptococci, meningococci, mycoplasmas), entering a child’s body under comfortable conditions (for example, reduced immunity), can cause various diseases. There are many varieties of pathogenic microorganisms, as well as the infections they cause. When multiplying in the body, they release harmful toxins, and when they accumulate critically, the child shows the first signs of the disease - a temperature rise above 38 °C. The following symptoms are added:
- painful sensations in a certain place;
- deterioration of health, weakness;
- local enlargement and swelling of the lymph nodes;
- rashes on the skin, mucous membranes of the mouth, eyes.
Without drug treatment, the condition will rapidly deteriorate. If a bacterial infection is suspected, consultation with a doctor is required.
Viral infection
Often, on the first day of illness, children only experience an increase in temperature and nothing else. Some mothers begin to worry and want to find out the reasons for this phenomenon. But after a day, such characteristic symptoms of a viral infection are added as:
- sore or sore throat;
- runny nose, nasal congestion;
- cough;
- headache, muscle pain.
The child is advised to rest, drink plenty of fluids, eat sparingly, and receive adequate treatment from a doctor.
Overheat
In children under 5 years of age, the thermoregulation function works intermittently, so often under the influence of the following factors, the temperature can rise to 37-38.5 °C:
- walks under the scorching sun;
- long stay in a hot, stuffy room;
- long active games - running, jumping;
- wearing excessively hot, tight, uncomfortable clothing;
- tight swaddling.
In this case, headache, weakness, dry lips, cold extremities, decreased number of urinations, and red cheeks in the child may be observed.
If the factor that caused overheating is eliminated, the temperature and other accompanying symptoms return to normal within an hour.
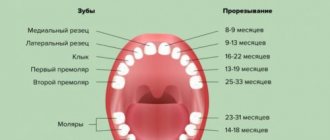
Teething
Often this process in children is accompanied by an increase in temperature to 39 °C. This is a natural reaction of the body. Children become restless, their sleep is disturbed, their appetite disappears, salivation increases, and their gums become swollen and red.
If your child has a high fever for several days, you should consult a doctor to rule out a possible infection.
Reaction to vaccination
Fever in children after vaccination is not considered a complication. Its slight growth is acceptable, since this is a reaction of the child’s body to the administered drug. Fever after vaccination may not appear immediately, but after several hours or days. Usually within 3 days the indicators return to normal.
If after vaccination a temperature above 39 °C is observed, the child should be given an antipyretic drug and contact a pediatrician.
Other reasons
In some situations, a child’s temperature can be caused by:
- inflammatory process of the urinary tract (pyelonephritis, pyelitis, ureteritis, cystitis, urethritis);
- stressful situations accompanied by strong feelings and excitement;
- metabolic disease;
- internal secretion disorders;
- benign or malignant neoplasms.
Why does the temperature rise during illness?
It must be remembered that high temperature during infection is a protective mechanism. In response to a virus or bacteria entering the blood, the cells of our body begin to produce pyrogens (substances that cause an increase in body temperature, fever). They stimulate certain parts of the nervous system responsible for thermoregulation. The nerve endings of these sections give the blood vessels a signal to contract. This is how the body retains the heat it already has. Therefore, a child with fever looks pale.
At this time, muscle tissue receives a signal for active work. This allows the body to produce more heat. That's why the baby is shivering. When the temperature reaches the optimal level, according to our nervous system, the body gives the command to dilate the blood vessels. The child's skin turns red, the shaking stops, and sweating begins. This happens at approximately 38.5-39°C. Why at these numbers?
Firstly, at this temperature, inflammatory mediators are produced - substances that fight infection in our body.
Secondly, high temperature prevents the growth of bacteria.
It turns out that a high temperature is not at all scary, and is even very useful during an infection. If the child tolerates the elevated temperature well, you can not rush to bring it down, but let the immune system fight the disease.
When is it necessary to “bring down” a child’s high fever?
1. If a child does not feel well, you should not try with all your might to maintain a high temperature. When the baby is capricious, cannot sleep, complains of a headache, body aches, then the temperature can be brought down. Moreover, in different situations and in different children, this condition can occur with different indicators on the thermometer.
2. There is a conditional criterion that the temperature should not be lowered below 38.5°C, and the temperature above this value must be “brought down”. Actually this is not true. Some babies do not tolerate temperatures of 37.5°C. Others feel quite tolerable even at 39°C. It is not so rare that I meet small patients who play calmly at 38.5°C and above.
3. If the baby has chronic diseases. For example: heart disease, metabolic disorders, neurological diseases. In such cases, there is a risk that an increase in temperature will worsen the course of the chronic disease. It is recommended for such children to “bring down” the temperature above 38-38.5°C.
4. Babies under 3 months of age are not recommended to wait until the temperature rises above 38-38.5°C.
5. If the child has previously had febrile seizures (a seizure that occurs in a child only when the child has a high temperature). Meeting such a patient at a pediatrician’s appointment is not uncommon. Usually this condition is benign and goes away on its own with age, without any treatment. It is recommended for such children to reduce their temperature to 38°C. Numerous clinical studies have proven that taking antipyretics prophylactically for such children (i.e., before the temperature begins to rise), repeating them regularly, regardless of the numbers on the thermometer, is not effective. In the same way as treating such babies with antiepileptic drugs.
6. If the temperature is above 41°C. This is the temperature that is considered critical and dangerous for the baby’s internal organs. With common infections, such figures are rare.
Appointment with a pediatrician
The doctor will examine the little patient and make the correct diagnosis, due to which the temperature rises to 39 in a child without symptoms. Lower temperatures have almost similar causes.
To determine the disease, the doctor will prescribe certain tests:
- Analysis of urine;
- blood analysis.
Based on the results, the pediatrician will be able to determine why the temperature rises in a 2-year-old child without symptoms.
One of the most common diseases can be these pathological processes:
- genitourinary tract infection;
- kidney diseases;
- manifestations of lesions in other organs of the internal system.
How to “bring down” a high temperature correctly?
- You should start by wiping with water slightly warmer than room temperature. In emergency cases with very high numbers, you should not be afraid of a cool shower. It is strictly not recommended to wipe children with alcohol solutions or vinegar. The surface of a child's skin absorbs substances to a much greater extent than that of an adult. Treating the skin in this way can cause poisoning.
- The baby should be given enough water. A lack of moisture in the body reduces sweating. This means that the body cannot fully give off heat and overheats.
- Do not wrap a sick child tightly. If the baby is shivering, this does not mean that he is cold. Do not cover it with a thick blanket and wear many layers of warm clothing.
The room of a sick child should be cool - optimally no higher than 21°C. Otherwise, the body will not be able to give off heat fully.
If physical cooling methods are not effective enough. It makes sense to switch to using antipyretics.
How to properly use antipyretic drugs for children?
It should be clarified that antipyretic drugs in children are used only when there is already a high temperature. A course of treatment to prevent an increase in body temperature, for example 3 or 4 times a day, does not make sense. There are many trade names and dosage forms adapted for use by children:
- For babies under one year old, antipyretic in the form of suppositories is more suitable. It must be remembered that the effect of drugs in this form occurs somewhat later than that of drugs that are administered orally;
- syrups and solutions are produced for children over one year old;
- Children over 7 years old can already take medications in the form of tablets.
In the instructions for the drugs, a single dose of the drug is usually indicated on average for the age of the child. But it is more correct to calculate the dose not by age, but by weight. Different babies at the same age can vary significantly in weight.
You should know that when taking an antipyretic, the temperature should not reach normal levels. A decrease in temperature of at least 1 degree is considered effective. But, even if the temperature has decreased to a lesser extent, and the child’s well-being has improved, this is already a positive effect from taking an antipyretic.
Online consultation with pediatrician Olga Nikolaevna Tekutyeva
Registration online
During the consultation, you will be able to voice your problem, the doctor will clarify the situation, interpret the tests, answer your questions and give the necessary recommendations.
What medications should children not take to reduce fever?
Nimesulide is prohibited for use in children under 12 years of age. It has a pronounced toxic effect on the liver.
Analgin (metamizole sodium) causes a marked decrease in blood neutrophils, often causing anaphylactic shock. Analgin, unlike other antipyretics, is capable of sharply reducing body temperature to extremely low numbers (34-35°C). It can be taken only in special conditions, under the supervision of a doctor, in the form of injections.
Aspirin (acetylsalicylic acid) is strictly prohibited in children under 15 years of age due to the fact that it causes a severe complication with high mortality - Reye's syndrome.
In conclusion, I want to say that all children, sooner or later in their lives, encounter a high temperature. There is nothing wrong with this if you know how to properly help your baby.
What not to do when the temperature rises
- Do not undress your child or cool him or her with blows or rubs; fever is a natural and healthy response to infection. Hypothermia can lead to complications from the infection.
- Do not cover your baby with a warm blanket or wrap him up, as this may cause heat stroke. Just cover your baby with a sheet or light blanket.
- Do not give aspirin to children under 16 years of age. Absolutely never! This may be due to a rare but dangerous disease called Reye's syndrome.
- In children under one year of age, medications available in the form of rectal suppositories are recommended to reduce fever.
- Do not self-medicate. For young children, the dose of drugs and the frequency of their use should be calculated individually; the prescription can only be made by a doctor after diagnosis.