Can a child have a different blood type? – parents often ask. Let's deal with this in order.
Already in the nineteenth century, people knew about the existence of four groups. Scientists mixed different biomaterials and noted that the cells stuck together and formed clots. This indicated that the liquids that were mixed were somehow different from each other.
Today people use the AB0 classification. Based on it, 4 types of blood are distinguished. It all depends on the presence and combination of certain substances (antigens and antibodies) in it:
- the first group does not contain antigens, so it is encrypted with the number 0,
- if protein A is present in the cells, this is the second one,
- thirds have B agglutinogen,
- and when agglutinogens A and B are combined, they speak of the fourth group.
The question often arises: can a child’s blood type differ from the parents’ blood? Yes, maybe we will consider this issue below.
In addition to antigens A and B, all people have a special protein D in their plasma and red blood cells; depending on its presence or absence, blood is divided into two categories. If this protein is present, then the person is Rh positive (Rh+); if it is not, the person is Rh negative (Rh-). This indicator does not affect health in any way.
General principles of inheritance of characters.
Simply put, every trait in the body (hair color, eye color, blood type, Rh factor) is encoded by two genes.
In reality, the number of genes that determine the trait is much greater. For each trait, the child receives one gene from the mother, another from the father. In genetics, dominant and recessive genes are distinguished. The dominant gene is designated by a capital letter of the Latin alphabet, and in its presence the recessive gene, as a rule, does not manifest its properties. A recessive gene is indicated by a capital letter of the Latin alphabet. If for some trait an organism contains two identical genes (two recessive or two dominant), then it is called homozygous for this trait. If an organism contains one dominant and one recessive gene, then it is called heterozygous for this trait, and at the same time those properties of the trait that are encoded by the dominant gene are manifested. For example: A is a dominant gene that determines brown eye color and A is a recessive gene that determines blue eye color
Possible genotype options: AA - homozygote, brown eyes Aa - heterozygote, brown eyes aa - homozygote, blue eyes
Example 1:
wife AA - homozygous, brown eyes, both genes are dominant; husband AA - homozygous, blue eyes, both genes are recessive
When germ cells (egg and sperm) are formed, one gene goes into each germ cell (gamete), i.e. in this case, the female body forms two gametes containing one dominant gene each, and the male body forms two gametes containing one recessive gene each. When germ cells merge, the embryo receives one maternal and one paternal gene for this trait.
wife AA + husband aa Gametes: A A a a Child: Aa Aa Aa Aa
Thus, in this situation, 100% of the children will have brown eyes and be heterozygotes for this trait.
Example 2:
wife Aa - heterozygote, brown eyes husband Aa - heterozygote, brown eyes wife Aa + husband Aa gametes: A a A a child: AA, Aa, Aa, aa
In this case, the probability of having children with brown eyes (homozygotes) is 25%, heterozygotes are 50% with brown eyes, and blue eyes (homozygotes) are 25%.
Example 3:
wife Aa - heterozygote, brown eyes husband aa - homozygote, blue eyes Wife Aa + husband aa Gametes: A a a a Child: Aa, Aa, aa, aa
In this case, 50% of children have brown eyes and are heterozygotes and 50% have blue eyes (homozygotes)
What determines a child's blood type?
Knowing your blood type is very important, for example, if you have to have a blood transfusion. After all, sometimes there is no time to conduct a laboratory analysis and time ticks by in minutes. And if we are talking about a small child, then even more so, parents are simply obliged to know his blood type and Rh factor. That is why in maternity hospitals newborn babies are tested to determine their blood type and Rh factor.
But many parents, even before the baby is born, want to calculate using genetic formulas what blood type he will have. Sometimes this calculation can be made with 100% accuracy, and sometimes some deviations are possible. This can be done according to ordinary genetic laws, which make it possible to determine the hereditary gene. The dominant genes are genes A and B, and gene 0 is recessive. At conception, the baby receives a set of genes from the mother and a set of genes from the father. Depending on which of them turn out to be dominant and which are recessive, not only the baby’s blood type will depend, but also many other signs and characteristics.
Patterns of inheritance of blood group and Rh factor.
Inheritance of blood type is controlled by an autosomal gene. The locus of this gene is designated by the letter I, and its three alleles by the letters A, B and 0. Alleles A and B are equally dominant, and allele 0 is recessive to both of them. There are four blood types. The following genotypes correspond to them: First (I) 00 Second (II) AA; A0 Third (III) BB; B0 Fourth (IV) AB
Example 1:
wife has the first blood group (00) husband has the second blood group and is homozygous (AA) wife 00 + husband AA gametes: 0 0 A A child: A0 A0 A0 A0
All children have a second blood group and are heterozygotes for this trait.
Example 2:
wife has the first blood group (00) husband has the second blood group and is a heterozygote (A0) wife 00 + husband A0 gametes: 0 0 A 0 child: A0 A0 00 00
In a given family, in 50% of cases it is possible to have a child with a second blood group, and in 50% of cases the child’s blood type will be first.
Inheritance of the Rh factor is encoded by three pairs of genes and occurs independently of the inheritance of blood type. The most significant gene is designated by the Latin letter D. It can be dominant - D, or recessive - d. The genotype of a Rh-positive person can be homozygous - DD, or heterozygous - Dd. The genotype of a Rh negative person may be dd.
Example 1:
wife has a negative Rh factor (dd) husband has a positive Rh factor and is a heterozygote (Dd) wife dd + husband Dd gametes: dd D d child: Dd Dd dd dd
In a given family, the probability of having a Rh-positive child is 50% and the probability of having a Rh-negative child is also 50%.
Example 2:
wife has a negative Rh factor (dd) husband has a positive Rh factor and is homozygous for this trait (DD) wife dd + husband DD gametes: dd DD child: Dd Dd Dd Dd
In this family, the probability of having a Rh-positive child is 100%.
Blood group combination
A child's blood type is inherited from his parents, but does it have to match? The answer is clear - no. It all depends on whether the parent has dominant genes and how they are combined at the time of conception. If they are carriers of the same proteins, the percentage that the baby will develop a different set of antigens is less. If the genes are different, the possibility that the fetus will have a completely different set of agglutinogens increases. Thus, we can only predict what composition will be passed on to children.
Read also: Preparation for CPK analysis, evaluation of results, norms and deviations
Many fathers and mothers wonder whether the child’s blood type can be different from the blood type that the parents have? After consulting with a doctor or studying certain literature, they understand that this is a completely normal phenomenon.
Features of the course of pregnancy with Rh factor incompatibility. Rhesus conflict.
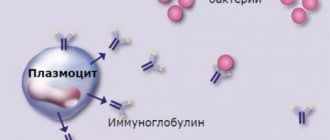
Hemolytic disease of the fetus and newborn is a condition that occurs as a result of incompatibility of the blood of mother and fetus for certain antigens. Most often, hemolytic disease of the newborn develops due to Rh conflict. In this case, the pregnant woman has Rh-negative blood, and the fetus has Rh-positive blood. During pregnancy, the Rh factor with the red blood cells of the Rh-positive fetus enters the blood of the Rh-negative mother and causes the formation of antibodies to the Rh factor in her blood (harmless to her, but causing the destruction of the fetal red blood cells). The breakdown of red blood cells leads to damage to the liver, kidneys, brain of the fetus, and the development of hemolytic disease of the fetus and newborn. In most cases, the disease develops quickly after birth, which is facilitated by the entry of a large number of antibodies into the baby’s blood when the integrity of the placental vessels is disrupted.
Less commonly, hemolytic disease of the newborn is caused by group incompatibility of the blood of mother and fetus (according to the AB0 system). In this case, due to agglutinogen (A or B), present in the fetal red blood cells but absent in the mother, antibodies to the fetal red blood cells are formed in the maternal blood. Most often, immune incompatibility manifests itself when the mother has blood group I, and the fetus has blood group II, and less often, blood group III.
The process of immunization of a pregnant woman begins with the formation of antigens in the red blood cells of the fetus. Since antigens of the Rh system are contained in the blood of the fetus from the 9-10th week of pregnancy, and group antigens - from the 5-6th week, in some cases early sensitization of the mother’s body is possible. The penetration of antigens into the maternal bloodstream is facilitated by infectious factors that increase the permeability of the placenta, minor injuries, hemorrhages and other damage to the placenta. As a rule, the first pregnancy in an Rh-negative woman, in the absence of previous sensitization of the body, proceeds without complications. Sensitization of the body of a Rh-negative woman is possible through transfusions of incompatible blood (carried out even in early childhood), during pregnancy and childbirth (if the fetus has Rh-positive blood), after abortions, miscarriages, and operations for ectopic pregnancy. According to the literature, after the first pregnancy, immunization occurs in 10% of women. If a woman with Rh-negative blood avoided Rh immunization after her first pregnancy, then during a subsequent pregnancy with an Rh-positive fetus, the probability of immunization again is 10%. Therefore, after any termination of pregnancy in a woman with Rh-negative blood, it is necessary to administer anti-Rhesus immunoglobulin for prophylactic purposes. During pregnancy, in a woman with Rh-negative blood, it is necessary to determine the titer of Rh antibodies in the blood over time.
Table of inheritance of blood groups in children from their parents
The most simplified option for determining the inheritance of blood type by children from their parents is a special table. Indeed, to be able to solve genetic problems, you need special training, and to be able to use the table correctly, you only need to understand its meanings.
Using the table of inheritance of blood groups in children from their parents is very simple. Using the first vertical column, you need to find the combination of blood groups of the child’s father and mother that you need. For example, one parent has a second blood group, the other has a third. We find a cell that displays the combination of sum II+III. From this cell we draw a horizontal line and find possible variants of the child’s blood groups. As can be seen from the above example, when combining the sum II + III, the child can have both the first, second, third, and even fourth blood group with the same percentage of probability.
Let's take another example. Both parents have the second blood group, i.e. combination of sum II+II. We find the cell we need and draw a horizontal line from it. We get the result: a child can have the first blood group with a probability of 25% and the second blood group with a probability of 75%.
With a 100% probability, the child will inherit only the first blood group, provided that both the mother and father also have the first group. The Rh factor has no effect on the inheritance of blood type.
The compatibility of the blood groups of the parents, as well as Rh factors, is often used to determine the optimal time for conception, since the blood groups of the father and mother do not have any obstacle to planning a pregnancy. But incompatibility of the Rh factor can present unpleasant surprises to a couple and even cause their infertility.
Of course, when using genetic calculations, the result will be more accurate and detailed. This can be seen from the table above.
Question 2:
I have a negative Rh factor. I recently had an abortion. Will I be able to have children? Is there a chance that the baby will be sick during the next pregnancy?
Answer
: The presence of a negative Rh factor does not directly affect conception. During an abortion (if it was performed at 9-10 weeks of pregnancy), there was a possibility of sensitization of the body to the Rh factor. Before a planned pregnancy, it is advisable to do a blood test for the presence of antibodies to the Rh factor.
Question 3:
What dose of anti-Rhesus immunoglobulin and in what time frame is administered to a woman with Rh-negative blood after childbirth? Is it true that the administered dose of the drug should be increased after a caesarean section?
Answer
: Women with Rh-negative blood after childbirth are given anti-Rhesus immunoglobulin in an amount of 1-1.5 ml (200-300 µg) no later than 24-48 hours after birth for prophylactic purposes. During surgical interventions, transplacental bleeding may increase, and therefore the administered dose of anti-Rhesus immunoglobulin is increased by 1.5 times.