Ultrasound of the cervix is a standard examination during pregnancy, allowing to exclude the threat of premature birth. The purpose of the procedure is to determine the length of the cervix: it is this indicator that allows you to judge whether there is a risk for the mother and child.
The cervix holds the fetus inside the body. During pregnancy, it gradually shortens and opens, allowing the woman to give birth. However, if the length of this organ was less than normal from the very beginning, then this threatens not only premature birth, but also miscarriage.
Short cervix (SCI)
Pathological shortening of the cervix or isthmic-cervical insufficiency is the most common cause of termination of pregnancy (35% of all statistics).
The disease can occur unsystematically and painlessly, so it can only be detected by an examination by a gynecologist. But still, ICI is usually accompanied by the following symptoms:
- stabbing pain in the vaginal area;
- discharge of a small amount of blood from the vagina;
- feeling of discomfort, heaviness and pressure in the lower abdomen.
If your belly size is not normal...
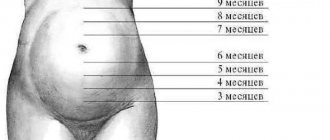
The rate of enlargement of the uterus, and therefore the growth of the abdomen, must quite strictly correspond to the above parameters, since they are an important indicator of the normal course of pregnancy.
In the early stages, when the uterus is not yet palpable through the anterior abdominal wall, the discrepancy between its size and the expected duration of pregnancy may be a sign of an ectopic pregnancy, while the fertilized egg most often develops in the fallopian tube.
Exceeding the expected size of pregnancy is characteristic of such a pathology as chorionepithelioma - a tumor that develops from placental tissue and represents a large number of small bubbles. With this tumor, the fetus dies, and timely treatment is necessary to preserve the health of the mother.
In later stages of pregnancy, a lag in the rate of increase in the uterine fundus most often occurs with fetal malnutrition, that is, with a delay in its growth. With this pathology, the baby is born even with timely birth with a weight of less than 2600 g, and its adaptation to extrauterine life is difficult.
Oligohydramnios in pregnant women can also cause the uterus to be smaller than expected. Among the possible causes of this complication are maternal hypertension, infectious and inflammatory diseases, inflammatory diseases of the female genital area, damage to the fetal excretory system, placental insufficiency, gestosis - a serious complication of pregnancy in which generalized vasospasm is observed; it is usually manifested by edema, increased blood pressure, and the appearance of protein in the urine.
A decrease in the height of the uterine fundus is possible with a transverse position of the fetus, when the baby in the uterus is positioned so that the head and pelvic end are on the sides. If the fetus is in a transverse position, delivery through the natural birth canal is impossible.
The size of the uterus is larger than the expected gestational age also occurs with multiple pregnancies. As you know, multiple pregnancy is a high-risk pregnancy: it increases the likelihood of various complications.
Will stretch marks appear during pregnancy? The skin on the abdomen stretches as pregnancy progresses. Will this process pass without a trace? It must be said that skin damage - so-called stretch marks - as a result of an increase in the volume of the uterus depends, of course, on the rate of growth of the abdomen, but for the most part their appearance is determined by the characteristics of the skin of the expectant mother. Of course, the likelihood of stretch marks slightly increases if the fetus is large, quickly gains weight, or if there is polyhydramnios, but the condition of the collagen and elastin fibers is decisive. To prevent stretch marks (striae), especially during intensive abdominal growth - in the third trimester of pregnancy - you can use products that improve skin condition. This is a special cosmetics for pregnant women, containing vitamins A, E, as well as substances that improve blood circulation in the skin. Since skin often becomes drier during pregnancy, you can also use moisturizing creams for pregnant women; they will also help prevent stretch marks. You can also prevent the appearance of stretch marks with the help of massage, which improves blood circulation in the skin. The technique of this massage is not complicated: you should stroke the stomach in a circular motion, pinching the skin along the periphery of the abdomen. If there is a threat of miscarriage, such a massage should not be performed, as it can provoke an increase in the tone of the uterus.
The uterus can enlarge with significant polyhydramnios - a condition when the amount of amniotic fluid exceeds the norm, reaching 2-5 liters, and sometimes 10-12. This pathology occurs in diabetes mellitus - impaired absorption of sugar, Rh-conflict pregnancy - when the body of a Rh-negative mother produces antibodies against Rh-positive erythrocytes of the fetus, in acute and chronic infections, and in fetal developmental anomalies. Of course, all these conditions require close attention from doctors.
The uterus may grow faster than usual if the fetus is large. In turn, a large fetus may be a consequence of both genetic characteristics and diabetes in the expectant mother during this pregnancy. A large fetus increases the risk of complications during childbirth, and diabetes requires treatment.
Thus, changes in the rate of increase in the height of the uterine fundus can serve as an indicator of various pathologies of the mother and, more often, the fetus. Therefore, if at the next appointment the doctor discovers that the height of the uterine fundus does not correspond to the gestational age, he prescribes additional studies to clarify the factors that caused the decrease or increase in the rate of abdominal growth.
Treatment of a short cervix
If there is a slight deviation from the norm, drug treatment is prescribed. This can be taking the drugs Magnesia and Ginipral, both intravenously and in the form of tablets. If this does not bring the desired results or the cervix is too short from the very beginning, then it is necessary to perform cervical cerclage - placing stitches on the cervix to keep the fetus inside. The sutures do not dissolve and are removed immediately before childbirth.
Sometimes the operation is replaced by the installation of an obstetric pessary. It can be installed later in pregnancy. This is a kind of bondage that serves the same purposes as sutures.
Ultrasound of the cervix is a simple and safe examination that can help you easily endure pregnancy and give birth to a healthy baby.
Assessment of the cervix during pregnancy using ElastoScan™ technology
Ultrasound scanner HS60
Professional diagnostic tools.
Assessment of tissue elasticity, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiological studies.
Introduction
Elastography is widely used for the diagnosis of tumors, as well as during biopsies of the liver, salivary, thyroid and prostate glands. The authors present preliminary data on cervical elastography assessment to demonstrate the utility of this method in assessing cervical consistency during pregnancy. Changes in the cervix on the eve of childbirth, otherwise called ripening, are accompanied by its softening towards the end of pregnancy. The presented images show the changes on the basis of which the authors concluded that it is possible to predict preterm labor and success in the case of induction of labor.
Methods
The presented illustrations, obtained using ElastoScan™ technology, show the cervix during pregnancy. B-mode echograms were obtained using Fetal Medicine Foundation criteria for measuring the internal os and cervical canal length. For elastography, color map 2 (with a scale from purple to red) was used. Fluid in the bladder or amniotic cavity is coded red, and fetal skull bones are coded purple.
The authors proposed the following scoring of images obtained using ElastoScan™: dense structures (purple color) were assigned 0 points, less dense structures (blue) 1 point, green - 2, yellow - 3, red - 4 points. Thus, a five-point scale called the Cervical Elastography Index (CEI) was formulated, and parts of the cervix (anterior and posterior lips, internal and external os, and cervical canal) were scored on the CEI.
In Fig. Figure 1 shows the immature cervix during pregnancy. The consistency of the cervix is the same in the area of the internal and external pharynx, cervical canal, anterior and posterior lips. All parts of the cervix shown in Fig. 1 were scored 0 points, which can be interpreted in two ways: the entire cervix is either firm or soft. After conducting about 50 studies, it was concluded that this picture corresponds to a rigid cervix without symptoms of ripening.
Rice. 1.
Cervix during pregnancy without signs of ripening.
A - internal os, B - external os, C - cervical canal, D - anterior lip, E - posterior lip.
In Fig. Figure 2 shows the cervix at a gestational age of 28 weeks, when the outer part of the lips of the cervix is softer than the area of the cervical canal. The anterior and posterior lip areas of the cervix were assigned a CEI score of 5, the external os a score of 2, and the midcervical canal a score of 3. At this time, the internal os of the cervix, the structure that plays the most significant role in the mechanism of maintaining pregnancy, was the densest part. The question arises whether this effect is the result of a softening of the cervical walls that occurs before ripening of the internal os begins, or the result of a hardening of the area of the internal os in response to increased pressure due to fetal growth.
Rice. 2.
Cervix during pregnancy with possible initial signs of ripening.
A - internal os, B - external os, C - cervical canal, D - anterior lip, E - posterior lip.
In case of impending labor (term or premature), the area of the internal os and the entire cervix become softer. The authors observed a statistically significant correlation between internal os CEI and success in inducing labor with oxytocin (r=0.71, p=0.0004). The softer the area of the internal pharynx, the higher the chances of a positive reaction to the administration of oxytocin. In Fig. Figures 3 and 4 show the cervix shortly before birth. Internal throat in Fig. 3 was scored 0 points, but the lower parts of the cervical canal - its middle and external pharynx - corresponded to 3 points.
Rice. 3.
The cervix shortly before birth.
A - internal os, B - external os, C - cervical canal, D - anterior lip, E - posterior lip.
In Fig. Figure 4 shows the cervix immediately before birth: the area of the internal os corresponded to 4 points on the CEI, similar to the middle part of the cervical canal, and was softer than the area of the external os (3 points).
Rice. 4.
The cervix just before birth.
A - internal os, B - external os, C - cervical canal, D - anterior lip, E - posterior lip.
It is difficult to assess the area of the internal os in patients with cervical incompetence. In Fig. Figure 5 presents a similar case, although the interpretation of this image requires further research.
Rice. 5.
Cervix during pregnancy with signs of cervical insufficiency.
A - internal os, B - external os, C - cervical canal, D - anterior lip, E - posterior lip.
The authors believe that changes in the elastographic picture of the cervix when examined using ElastoScan™ technology are so obvious that identifying the condition of the internal os area is more than 1 point according to CEI, as well as assessing the entire cervix, similar to that shown in Fig. 3 and 4 can be an easy and valuable prognostic sign of the onset of term or premature labor. Examination of the cervix using ElastoScan™ technology can be a method of objectively assessing the maturation of the internal os before term or premature birth. Emerging standards for cervical properties detected by elastography during pregnancy may be useful in diagnosing the risk of preterm labor at an early stage and planning induction of labor with prostaglandins or oxytocin.
Literature
- Celik E.. To M.. Gajewska K.. Smith GC et al. (2008) Cervical length and obstetric history predicts spontaneous preterm birth: development and validation of a model to provide individualized risk assessment Ultrasound Obstet. Gynecol. 31: 549-54.
- Chao AS., Chao A., Hsieh PC (2008) Ultrasound assessment of cervical length in pregnancy. Taiwan J. Obstet. Gynecol. 47: 291-5.
- Bishop EH (1964) Pelvic scoring for elective induction. Obstet. Gynecol 24:266–8.
- Brown JS, Crombleholme WR (1993) Handbook of Gynecology and Obtetrics. Appleton and Lange; East Norwalk.
- Ross MG, Beall MH (2009) Prediction of preterm birth: nonsonographic cervical methods. Semin. Perinatot 33: 312–6.
- Wischnik A. Stocklein R., Wemer T. Z. (1999) Geburtshilfe Neonatol. 203:115-9.
- Kuwata T., Matsubara S.. Taniguchi N.. Ohkuchi A. et aL (2010) A novel method for evaluating uterine cewical consistency using vaginal ultrasound gray-level histogram. J. Perinat. Med. [Epub ahead of print]
- Lang CT, Iams JD, Tangchitnob E.. Socrate S. et al. (2010) A method to visualize 3-dimensional anatomical changes in the cervix during pregnancy: a preliminary observational study. J. Ultrasound Med. 29: 255-60.
- Myers KM, Socrate S.. Paskaleva A.. House M. (2010) A study of the anisotropy and tension/compression behavior of human cervical tissue. J. Biomech. Eng. 132:021003.
- Berghella V., Baxter JK, Hendrix NW (2009) Cervical assessment by ultrasound for preventing preterm delivery. Cochrane Database Syst. Rev. 8: CD00723S.
- Aigner F., Mitterberger M., Rehder P., Pallwein L. et al. (2010) Status of Transrectal Ultrasound imaging of the Prostate. J. Endourol.
- Farrokh A.. Wojcinski S.. Degenhardt F. (2010) Diagnostic Value of Strain Ratio Measurement in the Differentiation of Malignant and Benign Breast Lesions. Ultraschall Med.
- Wojcinski S., Farrokh A.. Weber 5., Thomas A et al. (2010) Multicenter Study of Ultrasound Real-Time Tissue Elastography in 779 Cases for the Assessment of Breast Lesions: Improved Diagnostic Performance by Combining the Bl-RADS(R )-US Classification System with Sonoelastography.Ultraschall Med.
- Dighe M., Kim J., Luo S., Kim Y. (2010) Utility of the ultrasound elastographic systolic thyroid stiffness index in reducing fine-needle aspirations. J Ultrasound Med 29: 565-74.
- Bhatia KS, Rasalkar DD. Lee YP, Wong KT et al Evaluation of real-time qualitative sonoelastography of lesion focals in the parotid and submandibular glands: applications and limitations.
- Inoue Y.. Takahashi M.. Arita J.. Aoki T. et al (2010) lntra-operative freehand real-time elastography for small focal liver lesions: “Visual palpation” for non-palpable tumors. Surgery.
- Berzigotti A, Abraldes JG, Tandon P., Erice E. et al Ultrasonographic evaluation of liver surface and transient elastography in clinically doubtful cirrhosis. J. Hepatot [Epub ahead of print]
- Biswas R., Patel P., Park DW, Cichonski TJ et al. (2010) Venous elastography: validation of a novel high-resolution ultrasound method for measuring vein compliance using finite element analysis. Semin. Dial. 23: 105-9.
- Biswas R., Patel P., Park DW, Cichonski TJ et al. (2010) Venous elastography: validation of a novel high-resolution ultrasound method for measuring vein compliance using finite element analysis. Semin. Dial. 23: 105-9.
- Malgorzata Swiatkowska-Freund, Krzysztof Preis, Zofia Pankrac (2010) Ultrasound elastography in assessment of uterine cervical consistency during pregnancy. Archives of Perinatal Medicine 16(3). 175-177. 2010..
- Malgorzata Swiatkowska-Freund. Krzysztof Preis (2010) New methods of ultrasound examination of uterine cervix before labor induction, Gin Pol Med Project 2010; 3: (17), 9-15.
Ultrasound scanner HS60
Professional diagnostic tools.
Assessment of tissue elasticity, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiological studies.
The structure of the internal genital organs
- The vagina is a muscular organ whose boundaries are located between the cervix and the external opening. It is intended to receive the ejaculate of a man during the act of intercourse and becomes a passage for the fetus at the time of birth. The blood supply to this organ increases during pregnancy, as a result of which it acquires a bluish tint.
- The most important organ of the reproductive system, where the maturation of the fetus occurs, is the uterus. It is a hollow muscular organ and is shaped like a flattened pear. It can be divided into several departments:
- bottom. This is what they call the top part. It has a convex shape and is located above the line of origin of the fallopian tubes;
- body. The shape resembles a cone, which tapers at the bottom and forms an isthmus leading to the cervix;
- neck. Forms a kind of barrier between the uterus and the external environment. Designed to protect the woman and child from the effects of external infections and retain the fetus. Normally it is closed and begins to shorten a few days before birth.
- At the junction of the body of the uterus and the cervix there is an isthmus. The transition of the cervix to the isthmus is called the internal os, and in the vagina the cervical canal forms the external os.
- The fallopian tubes. Narrow passages attached to the uterus from above. They carry eggs from each ovary to the uterus.
- Ovaries. Paired organ in the form of an oval body. Is the female reproductive gland. Here, eggs are formed, from which, after fertilization, a new person grows. They also produce female sex hormones, which are responsible for the formation of female sexual characteristics.
Physiological role of cervix softening
During the process of bearing a child, the cervix remains dense for up to 32 weeks, its external os is closed. After this period, an uneven softening of the structure of the cervix occurs; it gradually “ripens” for opening during delivery. The cervix softens in the peripheral areas, the cervical canal itself remains closed, which is confirmed by ultrasound examination data.
How to prepare the cervix for childbirth
By the 36th week of pregnancy, the external pharynx allows the tip of the gynecologist’s finger to pass through during an examination in first-time mothers, and in women who become mothers again, the pharynx may be somewhat weaker, which is why it can allow the doctor’s entire finger to pass deeper.
From the 37th week, the cervix is already in a mature stage - it becomes soft, shortens, and during a medical examination the pharynx allows one or two fingers of the gynecologist to pass through. One of the reasons for such changes is that the fruit puts more pressure on the neck, which accelerates the process of its ripening.
Immediately before delivery, the cervix softens to such an extent that it is “smoothed” during labor to ensure the passage of the baby through the birth canal.
CIN 1 and pregnancy
Mild cell changes have virtually no effect on the course of pregnancy. In turn, the changes that occur in a woman’s body during pregnancy also do not have a strong impact on the development of the disease.
During gestation, the structure of the stratified epithelium undergoes physiological transformations characteristic of this period. The number of actively dividing cells increases, hyperplasia occurs and their differentiation changes. Therefore, when conducting diagnostics during pregnancy, the probability of obtaining false results is quite high.
If a woman is diagnosed with signs of mild dysplasia during pregnancy, the doctor will prescribe a colposcopy. Completing this examination does not affect the course of pregnancy, but if suspicion of cancer development is detected, the woman is referred to an oncologist.
If the cervix is in normal condition and no serious damage is observed, then the pregnant woman is recommended to undergo translational control examinations:
- Once every 30 days - colposcopy and cytology.
- 8-19 weeks after birth - re-examination.
- 3-4 months after birth - follow-up examination.
Depending on the test results, the doctor will select the optimal treatment method.
Is it possible to get pregnant
Women of childbearing age diagnosed with first-degree dysplasia often experience concomitant disorders, such as:
- Hormonal imbalances.
- Endometrial hyperplasia.
- Vaginal dysbiosis.
These factors can affect pregnancy and complicate conception. To normalize these conditions, combined oral contraceptives or Duphaston are prescribed. After eliminating these factors, problems with conception do not arise.
Treatment during pregnancy
Mild cervical dysplasia does not require treatment during pregnancy. This is due to the fact that the use of antiviral or immunostimulating drugs is not recommended during pregnancy. Therefore, when diagnosing dysplasia of the first, second or even third degree, doctors take an individual approach to the issue of treatment. Urgent measures are taken only if non-invasive or invasive cancer is suspected.
CIN 1 after childbirth
During pregnancy, a woman may experience signs of progression of the disease, but after the birth of the child these changes most often regress and only in rare cases worsen.
To monitor a woman’s condition after childbirth at 8-12 weeks, she is prescribed colposcopy and repeat cytology. If the condition is suspicious, a consultation with an oncologist may be scheduled.
With grade 1 cervical dysplasia, the prognosis after childbirth is positive. Weak changes caused by the influence of changed hormonal levels and decreased immunity, as a rule, regress after breastfeeding ends.
What is cervical LSIL and CIN 1
Mild cervical dysplasia is a collective term that refers to several types of precancerous conditions. Another name for the disease is cervical intraepithelial neoplasia or CIN.
Dysplasia is characterized by the occurrence of disorders at the cellular level. At the same time, the shape of the inner nucleus and the size of the cell change. Sometimes additional nuclei and vacuoles are formed. Damaged cells tend to divide rapidly, but do not extend beyond the mucous membranes. The disease progresses, affecting first of all the deep layers of tissue, and then the superficial ones. All changes occur secretly, the upper layers are visually unchanged at the initial stage.
There are 4 stages of the disease depending on the level of cell damage and the amount of deformation. Cervical dysplasia 1 is the initial degree, in which the changes are mild. They are observed in individual cells located only in the lower third of the epithelial layer. At the same time, the appearance and structure of the surface and intermediate layers remain normal.