ANTIBACTERIAL THERAPY OF ACUTE OTITIS MEDIA IN CHILDREN
L.S. Strachunsky, A.N. Bogomilsky
Children's Doctor, 2000, No. 2, pp. 32-33.
Epidemiology
Acute otitis media (AOM) is one of the most common diseases in childhood; occurs as a complication of respiratory bacterial and viral infections of the respiratory tract, most common in children aged 3 months to 3 years.
Etiology
The main bacterial pathogens of AOM are Streptococcus pneumoniae
and
Haemophilus influenzae
, less commonly –
Moraxella catarrhalis, Streptococcus pyogenes, Staphylococcus aureus
(Fig. 1).
The significance of Chlamydia pneumoniae
in the etiology of AOM is being clarified.
Sensitivity of pathogens to antibiotics
The sensitivity of AOM pathogens to antibiotics varies significantly in different regions. The general trend is an increase in the resistance of pneumococci to penicillin, macrolides, and Haemophilus influenzae to ampicillin and amoxicillin. Patients who have recently received courses of ampicillin, amoxicillin or penicillin are significantly more likely to isolate b-lactamase-producing microflora.
In the central part of Russia, S.pneumoniae
and
H. influenzae
isolated during AOM remain highly sensitive to aminopenicillins and cephalosporins: 97.0% of
S. pneumoniae
are sensitive to amoxicillin, 100% to amoxicillin/clavulanate and cefuroxime;
98% of H. influenzae
are sensitive to amoxicillin, 100% are sensitive to amoxicillin/clavulanate and cefuroxime.
The main problem is the high resistance of pneumococcus and Haemophilus influenzae to co-trimoxazole: resistance was observed in 35% of S.pneumoniae
and
H. influenzae
.
Indications for prescribing antibacterial therapy
When a child is diagnosed with AOM, it is necessary to answer the main question: “Is there a need to prescribe an antibiotic?” First of all, the picture of the disease is taken into account.
For moderate and severe cases, antibiotics are almost always used, especially in children under 2 years of age. In children over 2 years of age, in the absence of pronounced symptoms of intoxication, pain, or body temperature above 38oC, during the day one can limit oneself to only symptomatic therapy. However, if there is no positive dynamics in the symptoms of the disease within 24 hours, it is necessary to begin antibacterial therapy.
It should be borne in mind that it is well known that in 60% of cases, AOM resolves without the use of antibiotics. This is typical for AOM in children over 2 years of age with a favorable background, from prosperous families, when the disease is caused by viruses or Haemophilus influenzae.
Choice of antibiotics
It is advisable to select empirical therapy for AOM based on regional data on the prevalence of clinically significant pathogens (Fig. 1) and their sensitivity to antibiotics, taking into account the severity of the child’s condition. Unreasonable antibacterial therapy contributes to the development of bacterial resistance to antibiotics and adverse drug reactions.
For new-onset AOM or in children who have not received antibiotics during the previous month
(Table 1):
| In case of AOM in children who have received antibiotics during the previous month, in frequently ill children, in case of ineffectiveness of amoxicillin after 3 days of use (Table 2):
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Otitis
Do people's ears often hurt?
Inflammation of the middle ear - acute otitis media (AOM) - occurs in up to 62% of children already in the first year of life!!! During the first five years of life in the United States and Western Europe, more than 90% of children experience at least one NDE, which means we need to know how to help ourselves and our children with the development of such a frequent and unpleasant disease.
What is the reason?
No doctor will tell you with certainty what is the cause of otitis media. It is believed that this is more often an infectious disease that can be caused by a virus, bacteria or fungus. This can also be a manifestation of an allergic reaction and occur for other reasons. Otitis is a frequent companion to acute respiratory infections, especially with a severe runny nose. Snot, flowing down the back wall of the pharynx, carries the infection into the auditory tubes, and through them it enters the middle ear. This is how inflammation occurs.
Has your ear blown?
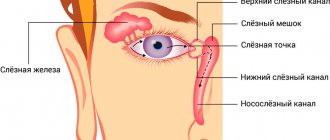
It is a common belief that your ear can hurt if you blow into it! Can't inflate in the ear. Otitis is not a contagious disease and does not occur from wind and cold. It cannot be prevented by regularly wearing a hat or wrapping the ear. The middle ear is completely isolated from the external environment by the eardrum, which does not allow air or bacteria to pass through. The infection enters the middle ear from the nasopharynx, since the middle ear is connected to the nasal cavity by a hollow cartilaginous tube - the Eustachian tube.
Different otitis media: AOM or ESO?
Normally, the Eustachian tube opens when swallowing, and through it mucus from the inner ear flows into the nasopharynx (have you heard the clicking sound in your ears when swallowing? - the tube opens!). When there is inflammation in the nose, the mucous membrane of this tube swells and blocks the exit of mucus from the middle ear, the ear is bursting with accumulated mucus and sharp pain is observed, there is dizziness, vomiting, high (up to 40) temperature and even decreased hearing. But this is not yet acute otitis media, it is called acute exudative otitis (ESO), sometimes this otitis is called tubootitis or eustacheitis. It lasts on average 48 hours. It may go away on its own, or if the accumulated mucus becomes infected, it may be complicated by acute otitis media.
Are we eating antibiotics?
Otitis media is one of the leading reasons for the prescription of antibiotics, often unjustified. In France, more than 3 million and in the United States about 30 million prescriptions for antibiotics are written annually for acute otitis media.
But is it necessary to take antibiotics if otitis media occurs?
Not always. There are publications showing that antibiotics have no effect at all on recovery from otitis media. And why, one might ask, poison the body? But in a real situation, it is necessary to take into account the likelihood of developing complications of otitis, and these complications are as follows: perforation (that is, a hole) of the eardrum, adhesion (gluing) of the auditory ossicles or their destruction, brain abscess, meningitis. That is why it is impossible to unequivocally refuse antibiotics for otitis media.
But you need to know that:
Antibiotics are indicated only for AOM, but should not be used for EOM (tubo-otitis), that is, in the first 48 hours after the onset of the disease, if a person has a viral disease, i.e. ARVI, then antibiotics are even harmful, they will weaken the immune system and cause allergization. The diagnosis of AOM requires confirmation of the presence of effusion in the middle ear, that is, if, during examination by an ENT doctor, a hyperemic and bulging eardrum is noticed, in combination with acute local manifestations (severe pain) and general symptoms (dizziness, vomiting, temperature), then this is truly acute otitis media and here you need to take antibiotics (not for otitis, but for possible complications!)
We treat ourselves
How can we help ourselves or our child with acute pain in the ear when otitis suddenly begins? Firstly, you need to provide the child with bed rest and rest, especially if he has a fever. It is necessary to lay the child with the sore ear up and drop a few drops of Otipax there (if there was no perforation of the eardrum before!), give the child an anesthetic (Panadol, Efferalgan or Nurofen in syrup for children, in a dose appropriate to the age and body weight of the child ( according to the instructions), drop a few drops of a diluted solution of “dolphin” or aqua-maris into the nose (the previously fashionable vasoconstrictor drops give a temporary and not radical effect, and after them there is often a “recoil” effect - the nose becomes even more stuffy, so these remedies are without It is better not to use urgent doctor's recommendations!) and give the child to chew the child's orbit. Yes, yes, give him chewing gum! Let him chew it 4-6 times a day during the entire illness with otitis media. This will lead to the opening and cleansing of the auditory tubes, possibly and to a quick recovery. Chewing gum is so useful for runny nose and otitis media that there may be talk of an alternative to antibiotics! Xylitol (xylitol), a natural 5-hydroxy alcohol contained in chewing gum, has been shown to inhibit in vitro the growth of bacteria Streptococcus mutans and S. pneumoniae. Using chewing gum (5 times a day) with xylitol reduces the incidence of acute otitis media in children by 1/3! And of course, the child must be shown to an ENT doctor. After all, it is he who can, upon direct examination, determine what kind of otitis media a patient has - exudative or already moderate?! And better, earlier. If a doctor is not available, Otipax drops should be instilled every 15 minutes 3 times, and then every 2-3 hours, and then less often, 3 times a day. These measures often save you from otitis media in 1-2 days than waiting a long time for the doctor to come or for you to get an appointment with him. It is also useful to have a blue glass lamp at home (a regular blue light bulb 60-75 W) and screw it into a table lamp instead of the usual one to warm the child’s sore ear 1-2 times a day from a distance of 15-20 cm for 5 minutes for 7-8 days in a row. . If the measures indicated in this booklet do not help within 48 hours after the onset of acute pain, a doctor should definitely see the child! He will probably still have to take an antibiotic or undergo some kind of medical procedure.
How to avoid getting otitis media?
To avoid getting otitis media at all, you must not get a runny nose! Neither removal of enlarged adenoids (proven by research) nor antibiotic prophylaxis can prevent otitis media. Most often, otitis media occurs from improper nose blowing!
How to blow your nose correctly?
How to blow your nose incorrectly: they pressed a handkerchief over the child’s nose and said, “Blow!” He will blow, but only the entire infection will fly into the ears through the Eustachian tube. How to blow your nose correctly: do not pinch your child’s nostrils! No need to press the wings of your nose! Let him blow his nose once or twice like this (and just keep the handkerchief next to your nose, don’t touch your nose at all, wipe anything that might get a little dirty, gently wipe it off, for irritation under the nose for a long-term runny nose, use baby cream), and then you can blow your nose like this: one nostril was pressed, the child took in air with his mouth and blew his nose into the free nostril, then change the nostril. And if you immediately pinch the nostril or even press the wings of the nose, as many parents like to do when the child blows his nose, then he will probably suffer from otitis media.
An excursion into psychology
The human body, like a finely tuned musical instrument, sensitively reacts with every cell to changes in the psychological atmosphere around it. Children especially experience stressful moments in life with all their being. And there is an opinion that in those families where the child hears what he does not want to hear (swearing and screaming of parents, extremely emotional arguments between relatives, insults and insults, even “jokingly” inflicted on him or his mother, obscene expressions, swearing) Children suffer from ear diseases more often and more severely. Take care of your children, watch your speech and what the child hears. Don’t wrap your child up, toughen him up, develop him physically, teach him to keep his mouth closed, learn to rinse his nose yourself at home, and use antibiotics only as a last resort when it’s really necessary. Do not shift the concern about your future to the doctor, think about the health of your children yourself, and you will succeed!
THERE ARE CONTRAINDICATIONS - YOU MUST CONSULT A DOCTOR