Types of analysis
The analysis has no variations and is carried out using the Benedict method.
Most often, stool testing for carbohydrate content is carried out on young children (up to one year of age), with its help the diagnosis of “lactase deficiency” is confirmed (poor digestibility of milk and products containing lactose - milk sugar - by young children). Due to the fact that breast milk or formulas containing milk sugars are the main product consumed by infants, lactase deficiency poses a serious threat to the health of the baby.
Indications for the study in young children:
- Increased regurgitation in an infant.
- Bloating.
- Signs of increased gas formation in the intestines.
- Pain in the abdomen.
- Flatulence.
- Insufficient body weight gain.
- The presence of foamy, liquid, sour-smelling stool.
Occasionally, analysis is prescribed to adults. If an adult has experienced abdominal pain, flatulence and discomfort for a long time in the absence of diseases of the gastrointestinal tract (gastrointestinal tract), he may also be prescribed a stool test for carbohydrates.
Causes of lactase deficiency
Lactase is an enzyme secreted by the pancreas and involved in the breakdown of lactose; its deficiency can develop in two cases, which occur in children in the first year of life:
- Immaturity of the pancreas.
- Development of intestinal dysbiosis.
Decoding the analysis results
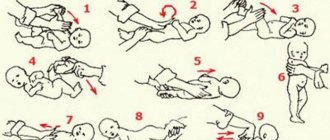
In children under one year of age, the normal carbohydrate content in feces ranges from 0% to 0.25%. Carbohydrate content from 0.3% to 0.5% is considered a slight deviation from the norm, from 0.6% to 1% - average deviations, over 1% - significant deviations. Lactase deficiency requires complex therapy, including correction of microbiological abnormalities, a strict diet for a nursing mother and massaging the tummy.
Norm of carbohydrates in feces
| Patient age | Amount of carbohydrates |
| Children under 1 year | 0 – 0,25% |
| Children over 1 year old and adults | Not detected |
Note: in children of the first year of life the following deviations from the norm may be observed:
- 0.3 – 0.5% (insignificant);
- 0.6 – 1% (average);
- more than 1% (significant).
Factors influencing the result:
- Violation of the rules for preparing for analysis;
- Errors when collecting biomaterial;
- Features of the daily diet;
- Patient's age;
- Genetic factors and family history;
- Intestinal infection or inflammation;
- Taking prebiotics, antibiotics and other drugs.
Reasons for deviations
Exceeding the permissible amount of carbohydrates in feces is characteristic of lactase deficiency; in addition, this may indicate a violation of the absorption of other sugars. The analysis may show a false positive result if the child shortly before took ascorbic acid, antibiotics, salicylates, or other drugs. In addition, an unreliable result can be obtained if the child ate a low-lactose formula before the analysis.
If there are low or moderate deviations from the norm in the carbohydrate content in the child’s feces, the patient continues to be monitored and, over time, an acidity test and another study are prescribed. If the carbohydrate level is above 1% and a certain clinical picture is present, the baby is diagnosed with lactase deficiency and treatment is prescribed. The carbohydrate content of stool may be explained by the presence of other pathological factors, including:
- chronic pathologies of the small intestine, including Crohn's disease (inflammation of the gastrointestinal tract of the granulomatous type), celiac disease (lack of correct breakdown of gluten);
- secondary malabsorption of an acquired type (develops after intestinal infections, operations on the gastrointestinal tract);
- acquired deficiency of the sucrose-isomaltase complex, which is expressed by dyspepsia (disturbance of the digestive process) after eating cereals, products with malt, starch.
Feces for carbohydrates
The food that a person eats includes fats, proteins and carbohydrates. Carbohydrates are the main source of energy necessary for the body to function. In food they can be represented by mono-, di-, oligo- and polysaccharides. Complex carbohydrates (polysaccharides) are chains of simple sugars connected to each other (glucose, sucrose, fructose). Their digestion occurs with the participation of enzymes of gastric juice, pancreas, intestines, and bile. The breakdown of complex carbohydrates into simpler ones begins in the oral cavity and continues in the gastrointestinal tract. The splitting process occurs gradually. Its last stage is the hydrolysis of disaccharides to monosaccharides and their absorption in the small intestine. The body may react inadequately to some foods due to complete or partial intolerance. This is observed in cases:
a) congenital (due to mutation of genes responsible for the production of enzymes) enzyme deficiency;
b) acquired enzyme deficiency caused by:
- pathologies of the small intestine (in particular, celiac disease - intolerance to the cereal protein gluten, Crohn's disease - a chronic recurrent inflammatory bowel disease);
- other diseases of the digestive tract (for example, pancreatitis);
- acute intestinal infections.
Any of the pathologies is accompanied by impaired absorption (malabsorption) of carbohydrates. The deterioration of a person’s well-being is caused by an excess intake of carbohydrates with a lack of enzymes for their processing. As a result, sugars that are not completely broken down enter the large intestine, where they become food for microbes that live in large quantities in this section. There the final breakdown of complex sugars into simple components occurs, but the absorption process is disrupted. In addition, bacteria produce excess gases - hydrogen and methane. Impaired malabsorption in combination with increased gas formation manifests itself:
- bloating;
- stabbing pains;
- excessive release of gases;
- watery diarrhea.
Data from recent studies also give reason to assume that impaired absorption of carbohydrates is one of the causes of the development of depression, headaches and a number of other diseases; the causes of their occurrence and development have not been established. The most poorly tolerated carbohydrate is milk sugar (or lactose).
One of the main purposes of this test is to identify lactase deficiency in children aged 0-12 months (a condition characterized by impaired absorption of lactose and poor tolerance to products containing milk sugar).
Lactose is the main carbohydrate found in milk. It contains glucose and galactose. The breakdown of lactose into its components occurs in the small intestine under the influence of the enzyme lactase. Undigested lactose residues, being in the intestinal lumen, retain fluid and provoke diarrhea, increased gas formation, and painful cramps in the abdomen. With lactase deficiency, the lactase enzyme does not show proper activity, which can be either a congenital or acquired condition. A manifestation of this pathology is lactose intolerance, i.e. the inability of the enzyme to break it down into monosaccharides. Another name for lactose intolerance is lactose intolerance.
This pathology most acutely affects young children, in whose diet dairy products predominate (and in children under one year of age they are generally the main food product). Of the total amount of carbohydrates contained in breast milk, the lactose content is 80-85% (6-7 g per 100 ml). Cow's milk contains less milk sugar - 4.5-5 g per 100 ml of product. In other dairy products its content is even lower.
During pregnancy, the enzyme appears at 10-12 weeks, increases activity from the 24th week and reaches a peak value at the time of birth. The enzyme exhibits the greatest activity in the middle section of the small intestine (jejunum), but then it levels out along the entire length of the intestine. Compared to 28-34 weeks, lactase activity increases threefold by 39-40 weeks. The last weeks of pregnancy are characterized by a rapid increase in enzyme activity, which at this stage exceeds the level of activity of adults. Based on the above facts, we can conclude that lactase deficiency is characteristic of premature and immature children at the time of birth. The activity of lactase during the neonatal period is 2-4 times higher than the activity of the enzyme in children 10-12 months old. In the process of growing up, it further decreases. The activity of the enzyme in the adult body decreases by 10 or more times compared to the first months of human life.
Latcase deficiency has a gradation depending on:
- depending on the severity - it can be partial (hypolactasia) or complete (alactasia);
- from origin - primary (a congenital form of reduced enzyme activity without damage to the cells of the surface tissue of the intestine - the enterocyte), and secondary (associated with disorders of the enterocyte).
In turn, primary lactose deficiency is divided into:
- to congenital (caused by changes at the genetic level, family);
- to transient (characteristic of premature and immature children at the time of birth);
- for lactose deficiency of the adult type (constitutional, characterized by a decrease in lactase activity by the end of the first year of life and further progress of this process).
Secondary lactose deficiency is typical for children under one year of age. It can be observed:
- with intestinal dysbiosis;
- with immaturity of the pancreas;
- with rotavirus;
- with opportunistic microflora;
- for food allergies;
- in case of digestive disorders (celiac disease);
- with giardiasis;
- with enteritis (chronic inflammation of the small intestine).
In young children, the nature of lactose deficiency is often secondary, transient (i.e., passing over time). Its manifestations are colic, restless behavior, dyspeptic disorders (impaired functioning of organs involved in digestion). When the manifestations of the underlying disease and lactase deficiency overlap, it is very difficult to diagnose it. As the baby grows and the intestinal microflora is corrected, secondary lactase deficiency goes away on its own, and the body subsequently absorbs lactose normally. To confirm or refute the presence of lactase deficiency, a stool test is performed using the Benedict method, through which the body's overall ability to absorb carbohydrates is determined. Within the framework of this technique, a reaction is carried out to identify sugars capable of reducing copper from the Cu2+ state to the Cu1+ form (i.e., sugars with reducing activity), namely glucose, galactose, maltose, fructose. Sucrose does not have this property. The normal content of such sugars in feces is low. If the indicators obtained as a result of the study are higher than the reference ones, it means that there is a violation of the process of breakdown and absorption of sugars. Examination of children under one year old allows detection of lactose residues in the stool, as well as galactose and glucose - products of its breakdown by the microflora of the large intestine and excrement. Identifying individual types of disaccharidase deficiency using this method is impossible, but it is quite applicable for the initial examination and monitoring the correctness of the recommended diet.
How the research works
The basis for prescribing a stool test to detect dysbiosis is a medical indication. Especially if the doctor wants to get acquainted with the full composition of stool. During the examination, there is a need to check if there are any doubts regarding the occurrence and development of carbon deficiency in the infant under study.
To do this, the following unpleasant phenomena will have to be observed :
- flatulence occurs frequently;
- the occurrence of abdominal pain;
- burps quite often;
- diarrhea appeared;
- gaining weight very poorly;
- when other similar symptoms appear related to disorders associated with the absorption of various types of carbohydrates.
Carrying out a stool test for carbohydrates, relative to the norm, allows us to identify the presence of intolerance that has arisen in the baby.
To obtain an accurate result, careful preparation will be necessary. Doctors recommend not changing the infant’s feeding regimen, as this may show a deviation from the norm, demonstrating a false negative result when deciphering the data obtained for dysbacteriosis.
What portion of stool is considered normal for qualitative analysis? To obtain the result of an analysis for dysbacteriosis, you need to donate stool collected in the amount of one teaspoon. It must be delivered within 4 hours after the sample was taken. A stool test is performed for carbohydrates and dysbacteriosis after the baby has had a natural bowel movement. To collect stool, you need to use a clean container with a tight-fitting lid.
Preparing for analysis
To obtain reliable research results, the following preparation rules must be observed:
- 3 days before the analysis, exclude the use of rectal suppositories and cleansing enemas;
- a week before the procedure, stop taking medications: those that affect the character of stool (antidiarrheals, laxatives);
- increasing peristalsis (pilocarpine, belladonna);
- containing coloring pigments (barium, bismuth, iron, etc.);
- exclude colored (red and green) vegetables/fruits, juices from them, ketchup and tomato paste, alcohol from the diet;
A mandatory condition is not to undergo diagnostic tests with contrast (X-ray, CT, MRI, etc.) 2-3 days before the analysis.