The doctor prescribed antibiotics
If the doctor has prescribed antibiotics, and you are faced with a choice whether to treat the child with antibiotics or not, then you need to set priorities: what will happen if I start giving the child antibiotics, and what if I don’t give antibiotics?
Try to approach the issue intelligently, read the information, preferably from several sources. We need to weigh the pros and cons. But we must not forget about the main thing. It is imperative to remember that taking antibiotics must be accompanied by taking probiotics. It's the most important!
Unfortunately, these days there are often situations when parents ask the question: “I am treating my child with an antibiotic, but the doctor did not prescribe probiotics. What to do?". This is a serious question. Even 60 years ago, when no one talked about probiotics and their effect on the body was not proven, one could understand this situation. But not these days, when the effects of probiotics are already legendary!
The study of human microflora at the instigation of I. I. Mechnikov started at the beginning of the 20th century, but only in 2012 was large-scale work done on comprehensive monitoring of the human microbial community in all biotopes. The enormous role of the symbiotic microcosm in the functioning of the immune, digestive, nervous, hormonal and other systems has been proven.
It has been proven that the best probiotics are liquid probiotics with a high content of bifidobacteria and lactobacilli.
Harm or benefit
The attitude towards antibiotics is always ambiguous. I want to give the child only the best and safest. It should be remembered that the correctly chosen antibacterial drug is the key to a safe and uncomplicated way out of many unpleasant situations associated with bacterial infection.
The group of antibiotics today includes mainly semi-synthetic and synthetic drugs that kill bacterial cells or inhibit their growth. In addition to bacteria, certain types of antibiotics are also effective against fungi. But these drugs do not work on viruses.
Thus, a pediatrician prescribes an antibiotic to a child if he suspects a bacterial infection:
- in the ear,
- nose,
- respiratory tract,
- lungs,
- urinary system,
- less often in the gastrointestinal tract.
The main signs by which you can recognize the rampant bacteria are:
- purulent (green, yellow) discharge and
- persistent rise in temperature.
But some bacterial infections or fungi behave rather secretively and are detected only by laboratory or instrumental diagnostic methods (smears, cultures, blood tests: clinical, serology or PCR, x-ray of the lungs or paranasal sinuses).
When choosing an antibiotic, the doctor is guided by national recommendations, which specify which classes are safe for the child and effective against certain types of bacteria. More often, the choice falls on drugs with a wide spectrum of activity against most possible bacteria.
72 hours were allotted to evaluate the effectiveness of the drug . If during this time the child does not get better and a decision is made that the drug is ineffective, it will be changed to a second-line drug that is stronger and more resistant to the destructive action of bacterial enzymes.
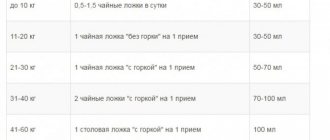
For the convenience of parents, the powder for preparing suspensions is available in several versions with different contents of the active ingredient per dosage spoon of the diluted drug.
The main mistake parents make is stopping the drug early, when the child gets better. The course of antibiotics is prescribed by the doctor, and its duration must be observed:
- For most drugs this is 7 days .
- Exceptions are cases when the drug has developed: an allergy (rash, swelling), in which case the use should be stopped immediately;
- If side effects occur, you need to consult your pediatrician.
Do children need antibiotics?
In some cases, there is no need to take antibiotics. Viral infections do not require the use of antibacterial drugs.
With the onset of the cold season, the percentage of RVI (rotavirus infection) infection increases. Unfortunately, in 80% of cases with RVI, children are prescribed antibacterial drugs.
The fight against the unjustified use of antibiotics is ongoing throughout the world. Advanced doctors say that antibiotic therapy is indicated only for real indications: for dangerous bacterial diseases, of which there are not many.
For a cold
What we call a cold (runny nose, clear snot, cough without phlegm, sore throat, hoarseness) does not require antibiotics even if there is a fever. The question about them will be raised if signs of bacterial infection appear (green snot, yellow sputum, temperature 38 or higher for more than three days).
Sometimes a child is affected by such formidable bacteria as meningococcus, when immediately after a short period of inflammation of the nasopharynx, against the background of fever, signs of damage to the nervous system and a rash appear in the form of many small bruises on the legs and buttocks. This requires an urgent call to the ambulance and the administration of antibiotics at the stage of examining the child by the team. Delay in this case could cost the child his life.
For the purpose of prevention, antibiotics should not be given to a child. They do not have a point of application until the bacteria are activated.
Different effects of antibiotics
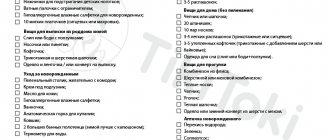
The effect of antibiotics on the intestinal flora varies, for example, Amoxiclav and Gentamicin act like napalm for the intestinal flora. Their tactics are “scorched earth tactics.” Taking these drugs must be accompanied by taking Bifidum BAG in double the daily dosage on all days of taking the antibiotic and then restoring the intestinal microbiocenosis according to the classic regimen of Bifidum/Trilact/Ecoflor. The drugs “Summamed”, “Klacid”, “Clarimycin” are more gentle on the intestinal microflora, but are also accompanied by taking a double daily dose of Bifidum BAG.
When are antibiotics not needed for children?
Despite the fact that the benefits of antibiotics are undeniable and often irreplaceable, there are conditions in which their use by both children and adults is completely inappropriate:
- viral diseases - this includes influenza, and other acute respiratory viral infections, and some cases of bronchitis, and other diseases of a viral nature; antibiotics are effective exclusively against bacteria and have no effect on the viral flora;
- fever - if the baby’s body temperature increases, then this is far from a reason to use antibiotics; this category of medications does not have an antipyretic, analgesic, or anti-inflammatory effect, but is exclusively antibacterial; at the same time, neutralization of the bacterial flora leads to the above effects, but only if the symptoms are caused specifically by bacteria;
- intestinal infections - acute intestinal infections in children, accompanied by watery diarrhea, cannot be treated with antibiotics; Consultation with a specialized specialist is strongly recommended;
- prevention of bacterial complications - often a bacterial disease develops against the background of a viral disease, for example, a cold or acute respiratory viral infection can develop into bacterial bronchitis, or otitis media, or even pneumonia in a matter of days; But giving antibiotics to children for preventive purposes is not only useless, but also harmful, since this also develops bacterial resistance.
The main contraindication to the use of antibiotics in children, which is most often violated, is ARVI. Respiratory viral infections can quickly develop into a bacterial infection. Even if it is still viral in nature, respiratory tract ailments can be confused with bacterial ones - both parents and doctors are susceptible to this. For example, it is very difficult to determine the nature of the infection in infants, and in very young children the addition of a bacterial infection occurs in the vast majority of cases already on the third day. As already noted, as part of prophylaxis, antibiotics are not prescribed for children , however, if the symptoms of the disease do not subside by the third day, there is a 99% probability of a pathogenic bacterial flora. This is indicated by the following symptoms of complicated ARVI:
- temperature 38°C at the age of up to 3 months and 39°C at the age of 3 years for 3 days or more;
- after the condition improves, a few days after the onset of the illness, on the 5-6th day, the symptoms return and also get worse;
- enlarged lymph nodes in the neck;
- prolonged cough for more than 10-14 days - there is a risk of whooping cough;
- purulent discharge from the nasal passages - there is a risk of sinusitis;
- white or purulent plaque on the tonsils - this can be a sore throat, scarlet fever, diphtheria, mononucleosis.
The above symptoms automatically transfer acute respiratory diseases from the category of contraindications to the category of indications for the use of antibiotics. In severe forms of acute respiratory infections, antibiotics are prescribed at the discretion of the physician, since the exclusion of bacterial flora in the pathological process cannot be ruled out.
Effect of probiotics
It is strictly necessary to accompany the intake of antibiotics with liquid active bifidobacteria Bifidum BAG. Prescribing a probiotic during antibiotic therapy is more justified than later.
When taking antibiotics, probiotics protect their own flora from side effects, preserve the composition and functions of the microflora, and prevent allergic reactions and antibiotic-associated diarrhea.
Bifidum BAG price is 90 rubles for one bottle with a large number of beneficial bifidobacteria, vitamins, amino acids and other useful substances.
Bifidum BAG 90 rubles is a small price for ten billion cells (10 in 10 = 10,000,000,000) of beneficial bacteria, each of which contributes to the overall healing effect of the human body.
Names of children's antibiotics for coughs
Only a doctor can choose a children's antibiotic for a cough. Popular groups of drugs for use at a young age are:
- Penicillins – eliminate respiratory tract infections, have high bioavailability, and are effective against intracellular pathogens. Common medications are Amoxicillin, Flemoxin Solutab, Ecobol, Ospamox, Augmentin, Amoxiclav.
- Macrolides exhibit minimal side effects and are indicated for use in patients over two years of age to eliminate pneumonia, pharyngitis, and sore throat. Representatives: Sumamed, Azithromycin, Clarithromycin.
- Cephalosporins - used in the form of injections for intramuscular or intravenous administration for sinusitis, otitis media, pneumonia, acute tonsillitis, bronchitis, and respiratory diseases. Representatives: Zinacef, Ceftriaxone, Zinnat, Ceclor, Suprax.
- Aminoglycosides - used only for bacterial pneumonia of a protracted nature, they cause great harm. These include Gentamicin and Amikacin tablets.
Suspensions
Children's antibiotics in cough suspension are used very widely. Popular groups and tools include:
- Tetracyclines disrupt protein synthesis in bacteria and prevent them from multiplying. Appointed after eight years.
- Aminopenicillins - antibiotics are prescribed from infancy. Representatives: Ampicillin, Amoxicillin. The latter can increase allergies, cause nausea, vomiting and dysbacteriosis, therefore it is contraindicated for asthma and dermatitis.
- Macrolides are modern agents with low toxicity. These include Azithromycin, Erythromycin, Macropen. Azithromycin is contraindicated in infants under six months old; it can cause diarrhea and nausea. Sumamed helps with cough, bronchitis, pneumonia.
- Fluoroquinolones are used when other drugs do not help. They are very effective, but have a negative effect on the intestinal microflora. These include Moxifloxacin, Levofloxacin.
Syrups
An antibiotic for dry coughs in children in the form of syrup will help effectively cope with diseases. Popular tools of this format include:
- Amoxicillin - from the group of penicillins, treats pneumonia, otitis media, pharyngitis. The granules dissolve in water to form a syrup. Children are supposed to take a quarter of a dessert spoon.
- Augmentin is a powder for preparing syrup based on amoxicillin and clavulanic acid. Indicated for use from three months, otherwise it may cause allergies
- Zinnat - granules for making syrup help with diseases of the ENT organs accompanied by cough. Used from 3 months at a dosage of 10 mg twice a day.
- Suprax is a cefixime-based antibiotic that helps with bronchitis in patients older than six months. The dosage is 2-4 ml per kg of body weight.
- Sumamed forte - contains azithromycin from the azalide group, which is successfully used for pneumonia, otitis, and pharyngitis. Indicated for patients older than 6 months at a dosage of 10 mg per kg body weight.
Pills
The doctor prescribes an antibiotic for severe cough in children in the form of tablets if the child is over 4 years old
The drugs have a bitter taste, so they must be given to children with caution so that they do not spit out the medicine. You can crush the tablets and mix them with jam, honey
Popular antibiotics for coughs in children:
- Flemoxin Solutab - contains amoxicillin trihydrate, taken 250 mg three times a day. Indicated for use at any age.
- Biseptol is a combined antimicrobial drug that can be used from three years of age and is indicated for obstructive bronchitis accompanied by complications.
Recommendations for taking antibiotics
It is recommended to take the drug strictly at the same time, strictly following the dosage schedule. If the child does not get better within 2 or more days, the treatment regimen must be reconsidered. The same applies to cases when the condition worsens or severe adverse reactions occur. Antibiotics for children under one year of age have several more rules for taking them:
- Complete the course of treatment. Do not interrupt or stop taking the drug without consulting a doctor.
- Refuse antibiotics if diagnostics have denied the presence of a bacterial infection.
- Take the suspension only with clean, non-carbonated water. Do not use milk, tea or juices.
- Do not combine antibacterial agents with antihistamines or antifungals without a doctor's prescription.
- Do not give antipyretic drugs at the same time. By reducing the fever, they create the illusion of recovery.
- Monitor the expiration date of the suspension. More often it is 5-20 days.
Levomycetin is an essential broad-spectrum antibiotic
Levomycetins are popular antibiotics that help quickly cope with infectious processes. The first representatives of this group had a rather meager spectrum of action; they eliminated only a narrow range of pathogenic organisms. With the development of medicine, such drugs have become more and more effective, and their spectrum of action has expanded.
Despite their wide spectrum of action, antibiotics show the greatest effectiveness in the fight against gram-positive bacteria.
Modern chloramphenicol 2, 3 and 4 generations have an extremely broad effect. The most popular drugs are Moxifloxacin, Levofloxacin and Gatifloxacin.
With their help, you will be able to quickly overcome:
- gram-positive organisms
: staphylococci, streptococci; - gram-negative organisms
: Haemophilus influenzae, Escherichia coli, Protea, gonorrhea, Pseudomonas aeruginosa; - into nutricellular pathogens
: mycoplasma, chlamydia, legionella.
It should be noted that many drugs are contraindicated for children under 18 years of age. Also, elderly people should take such medications with extreme caution, since the components of the medications can damage the structure of the tendons. Be sure to keep a list of antibiotics from this group.
Antibiotic prescription and side effects
When prescribing a drug, the pediatrician takes into account the weight and age of the baby. Almost always, only one antibiotic is prescribed. It can be in the form of tablets, suspensions, or powdered form - it depends on the child’s ability to use it.
Basic drugs
If the diagnosis is correct, it is permissible to treat the child with the following drugs:
- Amoxicillin is from the penicillin group. Prescribed for severe cough that occurs due to pneumonia or against the background of acute otitis media, pharyngitis. Indicated for use in children over one year of age. The release form is granules that need to be well dissolved in warm boiled water. Dosage – a quarter teaspoon of syrup. Cost – from 150 rubles.
- Augmentin is a drug with multidirectional effects. Approved for use by babies after three months of birth. Release form: powder. Effective in treating prolonged cough. Cost – from 250 rubles.
- Zinacef is a second generation drug. Prescribed for pneumonia of varying severity, acute and chronic bronchitis, and sinusitis. Release form: injection. Prescribed to children from 30 to 100 mg depending on weight. Before administration, the medicine must be diluted with water in accordance with the instructions in the instructions.
- Zinnat is a drug prescribed for diseases of the ENT organs and is approved for the treatment of children after three months. Release form: granules. Cost – from 200 rubles.
- Suprax - prescribed for the treatment of bronchitis and ENT organs. Allowed for children from six months. Release form: granules for making healing drinks. Cost – from 500 rubles.
- Ceftriaxone is a third generation drug. Can be prescribed from birth. The dosage is calculated according to the child's weight. It is not recommended for use in infants with jaundice. The course of treatment is no more than 4 days. Release form: injection. Cost – 20 rubles 1 ampoule.
- Sumamed Forte - from the azalide group. The active ingredient is azithromycin. Prescribed for pharyngitis, otitis, pneumonia. Approved for the treatment of children from six months. Release form: powder. The duration of treatment is no more than three days. Cost – from 250 rubles.
- Flemoxin. The base is amoxicillin. Very effective in treating colds caused by bacteria. Prescribed for the treatment of children aged two years and older. Release form: tablets. Cost – 250 rubles.
- Biseptol. Active ingredients: sulfamethoxazole, trimethoprim. The drug is prescribed for the treatment of colds in children from two years of age. Release form: tablets. Cost – from 40 rubles.
Consequences of use
If initial signs of the disease are detected, it is recommended to start treatment not with antibiotics.
Treatment of cough and runny nose with antibiotics in a small child may be ineffective if the correct dosage is not followed and if treatment is interrupted for some reason. An incorrectly selected medicine will also not bring a positive result.
The following antibiotics require special attention:
- chloramphenicol: taking even one tablet can cause aplastic anemia, so giving it to a child is prohibited;
- an antibiotic of the tetracycline group is contraindicated for children, as it can damage the enamel of the baby’s teeth;
- fluorinated antibiotics, such as Ofloxacin and Pefloxacin, can disrupt the process of joint formation.
Parents often think that antibiotics for coughs in children are the most necessary and effective remedy for a small child and they cannot cause any harm to the child’s body.
Of course, this opinion is erroneous, because, firstly, an antibiotic does not completely cure the disease without including additional drugs in the treatment regimen, and secondly, an antibiotic can disrupt the intestinal microflora and reduce the functioning of the immune system. If the antibiotic is selected correctly, the dosage is calculated correctly, and the prescribed dosage regimen is not violated, then a significant improvement in the condition can be noticed within a couple of days.
What are broad spectrum antibiotics?
Broad-spectrum antibiotics are universal bactericidal drugs that will help get rid of many diseases. Most often they are prescribed for the treatment of various infections, the causative agent of which remains unknown. They are also prescribed if a person has become infected with a fast-growing and dangerous virus. Such drugs are indicated as prophylaxis after major surgical interventions. Remember that not all cheap drugs are so bad.
| Group | A drug | Mechanism of action |
| Tetracyclines | Doxycycline, Tetracycline | Kills bacteria and has an antiviral effect |
| Levomycetin | Moxifloxacin, Levofloxacin | Antimicrobial, antifungal and antibactericidal |
| Semi-synthetic penicillins | Carbenicillin, Ticarcillin | Inhibits the synthesis of the pathogen cell wall |
| Cephalosporins | Ceftriaxone | Changes the activity of a virus that has entered the RNA |
| Rifampicins | Streptomycin, Amphenicol | Interferes with protein production |
| Carbapenems | Meropenem, Meropenem, Cyronem, Imipenem | Antibacterial and anti-inflammatory, prolonged action |